Table of Contents
A colonoscopy is one of the most reliable procedures to detect colorectal cancer and other digestive health conditions at an early stage. For people at average risk, doctors now recommend starting colonoscopy screening at the age of 45. Those with family history or medical conditions may need to start earlier. Understanding when to begin, how often to repeat, and what precautions to take ensures that patients can receive the full benefits of timely screening.
For many years, the recommended age to start colonoscopy screening was 50. In recent updates, major medical associations lowered the starting age to 45 years old. The change was prompted by a rising incidence of colorectal cancer in younger adults. By lowering the recommended screening age, doctors aim to detect and treat precancerous polyps before they progress.
This guideline applies to both men and women at average risk of colorectal cancer. Colonoscopy is considered the gold standard because it allows doctors not only to view the inner lining of the colon but also to remove polyps during the same procedure.
While 45 is the standard starting age, some people should undergo colonoscopy earlier. High-risk groups include the following:
Family history: A first-degree relative with colorectal cancer or advanced adenomas. Start at 40, or 10 years earlier than the relative’s age at diagnosis.
Genetic syndromes: Lynch syndrome or familial adenomatous polyposis (FAP) may require colonoscopy in the 20s or earlier.
Chronic conditions: Inflammatory bowel disease (Crohn’s disease or ulcerative colitis) warrants earlier and more frequent surveillance.
Other risk factors: Obesity, smoking, heavy alcohol use, and diets high in processed meat can increase risk.
Table 1: Average vs. High-Risk Colonoscopy Recommendations
| Risk Category | Starting Age | Frequency Recommendation | Notes |
|---|---|---|---|
| Average Risk | 45 | Every 10 years if normal | General population |
| Family History | 40 or 10 years before relative’s diagnosis | Every 5 years or as directed | Depends on relative’s age and findings |
| Genetic Syndromes (Lynch, FAP) | 20–25 or earlier | Every 1–2 years | Much stricter due to high risk |
| Inflammatory Bowel Disease | Often before 40 | Every 1–3 years | Interval depends on disease severity and duration |
 How Often Should Colonoscopy Be Done?
How Often Should Colonoscopy Be Done?After the first colonoscopy, future screening intervals are based on findings and personal risk factors. The goal is to balance effective cancer prevention with patient comfort and healthcare resources.
Every 10 years: no polyps or cancer detected.
Every 5 years: small, low-risk polyps found.
Every 1–3 years: multiple or high-risk polyps, or significant family history.
Personalized intervals: chronic inflammatory conditions or genetic syndromes follow stricter schedules.
Table 2: Colonoscopy Frequency Based on Findings
| Colonoscopy Result | Follow-Up Interval | Explanation |
|---|---|---|
| Normal (no polyps) | Every 10 years | Low risk, standard recommendation |
| 1–2 small low-risk polyps | Every 5 years | Moderate risk, shorter interval |
| Multiple or high-risk polyps | Every 1–3 years | Higher chance of recurrence or cancer |
| Chronic conditions (IBD, genetics) | Every 1–2 years | Strict surveillance required |
Colonoscopy is routine and generally safe, but certain precautions maximize safety and accuracy. Discuss your medical history, medications, and allergies with your clinician. Complications such as bleeding, infection, or perforation are rare, and medication management may be needed for blood thinners, antiplatelet agents, or diabetes drugs. Always follow medical advice rather than stopping medications on your own.
The procedure itself typically takes 30–60 minutes. Including preparation, sedation, and recovery, plan for 2–3 hours at the facility.
Take prescribed bowel-cleansing solutions the day before the procedure.
Follow a clear liquid diet (broth, tea, apple juice, gelatin) the day before.
Drink plenty of water to prevent dehydration.
Follow instructions exactly to avoid rescheduling due to poor prep.
Avoid high-fiber foods such as nuts, seeds, corn, and whole grains.
Avoid raw fruits and vegetables with skins.
Refrain from red or purple foods and drinks that can stain the colon lining.
Use a low-residue diet with easy-to-digest foods.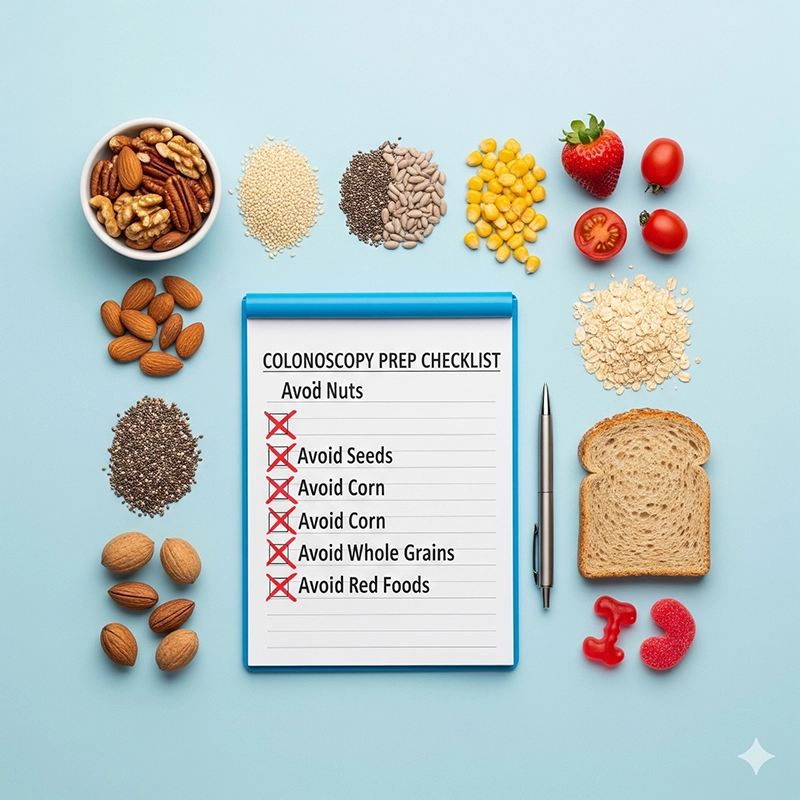
Expect 1–2 hours in recovery as sedation wears off.
Temporary bloating or gas is common due to air used during the exam.
Arrange a ride home; avoid driving for the rest of the day.
Return to normal activities the next day unless advised otherwise.
Report severe abdominal pain or persistent bleeding to a doctor.
There is a point when risks may outweigh benefits. Most guidance suggests individualizing decisions between ages 76–85 based on health, life expectancy, and prior results. For those over 85, routine screening is generally not recommended.
Early detection of precancerous polyps.
Prevention of colorectal cancer through polyp removal.
Improved survival when cancers are found at earlier stages.
Peace of mind for individuals with risk factors or family history.
By beginning colonoscopy at the right age, following risk-based intervals, and observing proper precautions, individuals can protect themselves against a highly preventable cancer while optimizing safety and comfort throughout the process.
Current guidelines recommend starting at age 45 for adults with no specific risk factors. This adjustment from 50 to 45 reflects the rise in colorectal cancer among younger populations.
For average-risk patients with normal results, every 10 years is sufficient. If low-risk polyps are found, every 5 years is recommended, while high-risk findings may require follow-ups every 1–3 years.
Individuals with a family history, genetic syndromes such as Lynch syndrome, or chronic conditions like ulcerative colitis should begin colonoscopy earlier, often at age 40 or younger, with shorter screening intervals.
Patients must follow strict bowel prep instructions, avoid certain foods five days prior, and inform their doctors about medications such as blood thinners or diabetes treatments to prevent complications.
Early detection of polyps, prevention of colorectal cancer progression, reduced mortality rates, and peace of mind for patients at risk are the key benefits of timely screening.
Copyright © 2025.Geekvalue All rights reserved.Technical Support:TiaoQingCMS