Table of Contents
A polyp in colonoscopy refers to an abnormal growth of tissue that forms on the inner lining of the colon. These polyps are usually discovered during a colonoscopy procedure, which allows doctors to directly view the large intestine. While many polyps are harmless, some can develop into colorectal cancer if they are not detected and removed. Colonoscopy remains the most effective method for identifying and treating colon polyps before they cause serious health problems.
Polyps are clusters of cells that grow in the colon or rectum. They can vary in size, shape, and biological behavior. Colonoscopy makes it possible to find polyps that cannot be detected through symptoms alone, as many polyps remain silent for years.
During colonoscopy, a flexible tube with a camera is inserted into the colon, providing a clear view of the intestinal lining. If a polyp is seen, doctors can remove it immediately through a procedure called polypectomy. This dual role of colonoscopy—detection and removal—makes it the gold standard in colorectal cancer prevention.
Polyps are significant findings in colonoscopy because they act as warning signs. While not all polyps are dangerous, some types have the potential to transform into malignant tumors. Detecting them early prevents disease progression
Not all colon polyps are the same. They can be classified into different categories based on their appearance and risk of becoming cancerous:
Adenomatous polyps (adenomas): These are the most common type of precancerous polyps. Although not every adenoma will develop into cancer, most colorectal cancers begin as adenomas.
Hyperplastic polyps: These are generally small and carry a low risk. They are often found in the lower colon and usually do not progress to cancer.
Sessile serrated polyps (SSPs): These look similar to hyperplastic polyps but are considered higher risk. If left untreated, they can develop into colorectal cancer.
Inflammatory polyps: Often linked to chronic bowel diseases such as Crohn’s disease or ulcerative colitis. They themselves may not be cancerous but indicate ongoing inflammation.
By classifying polyps correctly, colonoscopy guides doctors in setting proper follow-up intervals and preventive strategies.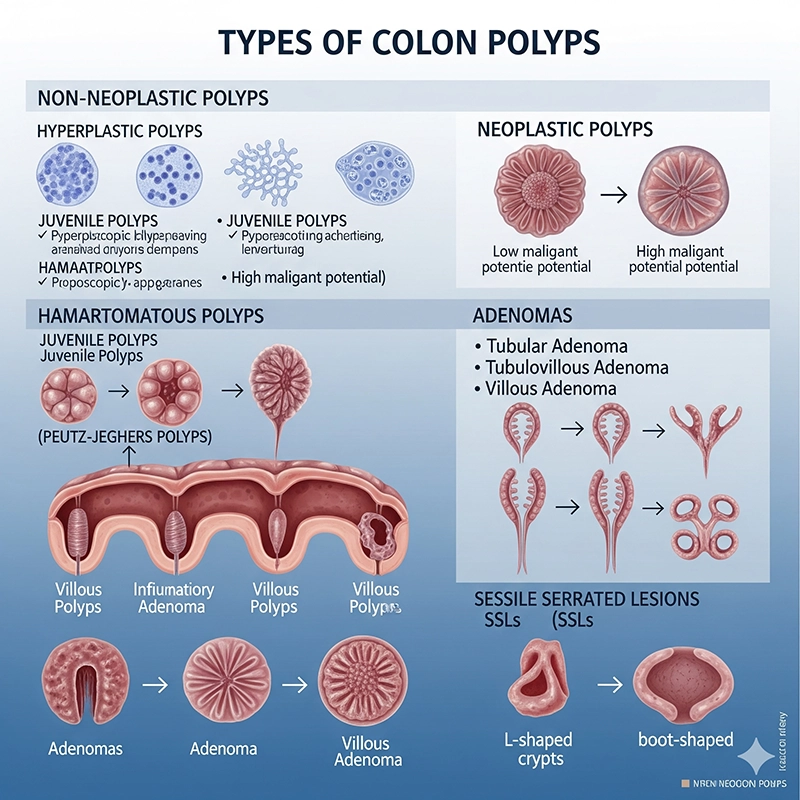
Several risk factors increase the chance of developing polyps that can be detected during colonoscopy:
Age: The likelihood of polyps increases after age 45, which is why colonoscopy screening is recommended at this age.
Family history: Having close relatives with colorectal cancer or polyps significantly raises the risk.
Genetic syndromes: Conditions like Lynch syndrome or familial adenomatous polyposis (FAP) predispose individuals to polyps at a younger age.
Lifestyle factors: Diets high in red or processed meat, obesity, smoking, and heavy alcohol use all contribute to polyp formation.
Chronic inflammation: Patients with inflammatory bowel disease (IBD), including Crohn’s disease and ulcerative colitis, are more likely to develop precancerous polyps.
Understanding these risks allows doctors to recommend colonoscopy at the right time and frequency.
Most polyps cause no symptoms at all. This is why colonoscopy is so important for early detection. However, when symptoms do appear, they may include:
Rectal bleeding: Small amounts of blood may be visible on toilet paper or in the stool.
Blood in stool: Sometimes stools may look dark or tarry due to hidden bleeding.
Changes in bowel habits: Persistent constipation, diarrhea, or changes in stool shape may indicate underlying polyps.
Abdominal discomfort: Cramping or unexplained pain may occur if polyps grow large.
Iron-deficiency anemia: Slow blood loss from polyps can lead to fatigue and anemia.
Because these symptoms can overlap with other digestive issues, colonoscopy provides the definitive way to confirm whether polyps are present.
One of the greatest advantages of colonoscopy is the ability to remove polyps during the same procedure. This process is known as a polypectomy. Small instruments are passed through the colonoscope to snip or burn away the polyp, usually without the patient feeling pain.
After removal, the polyp is sent to a pathology lab where specialists determine its type and whether it contains precancerous or cancerous cells. The results guide future management.
No polyps found: Repeat colonoscopy every 10 years.
Low-risk polyps found: Follow-up in 5 years.
High-risk polyps found: Repeat in 1–3 years.
Chronic conditions or genetic risk: Colonoscopy may be recommended as often as every 1–2 years.
This personalized schedule ensures that new or recurring polyps are caught early, greatly reducing cancer risk.
Colonoscopy is more than just a diagnostic tool. It is the most effective preventive strategy for colorectal cancer:
Early detection: Colonoscopy identifies polyps before they become symptomatic.
Immediate treatment: Polyps can be removed during the same procedure, avoiding future complications.
Cancer prevention: Removing adenomatous polyps significantly lowers the risk of colorectal cancer.
Public health impact: Routine colonoscopy programs have reduced colorectal cancer rates in many countries.
For patients, colonoscopy provides reassurance and control over their health. For healthcare systems, it is a proven method to save lives and reduce treatment costs by preventing advanced cancer.
A polyp in colonoscopy is a growth on the inner lining of the colon, often discovered before symptoms arise. While many polyps are benign, some have the potential to progress to colorectal cancer. Colonoscopy remains the best method for both detecting and removing these polyps, offering a powerful form of cancer prevention. By understanding the types of polyps, recognizing risk factors, and following appropriate screening schedules, individuals can protect themselves against one of the most preventable cancers.
A polyp is an abnormal growth on the inner lining of the colon. Most are benign, but some—such as adenomatous or sessile serrated polyps—can develop into colorectal cancer if not removed.
Colonoscopy allows direct visualization of the entire colon and enables doctors to detect small polyps that other tests may miss. It also allows immediate removal (polypectomy) during the same procedure.
The main types are adenomatous polyps, hyperplastic polyps, sessile serrated polyps, and inflammatory polyps. Adenomatous and sessile serrated polyps carry higher cancer risk.
Doctors perform a polypectomy using instruments inserted through the colonoscope to cut or burn away the polyp. The procedure is generally painless and done under sedation.
Follow-up depends on polyp type and number. No polyps means a 10-year interval; low-risk polyps require 5 years; high-risk cases may need 1–3 years. Patients with genetic risks may need checks every 1–2 years.
Copyright © 2025.Geekvalue All rights reserved.Technical Support:TiaoQingCMS