Table of Contents
A colonoscopy is an exam of the large intestine using a flexible video colonoscope that sends high-definition images to a monitor. In one minimally invasive visit, the doctor can look at the rectum and colon, remove polyps, take small tissue samples (biopsies), and stop minor bleeding. By finding and treating precancerous growths early—often before symptoms—colonoscopy lowers the risk of colorectal cancer and helps explain problems like bleeding or long-lasting bowel changes
Colorectal problems can grow quietly for years. A colonoscopic exam can spot tiny polyps, hidden bleeding, or inflammation long before pain or obvious symptoms appear. For average-risk adults, removing precancerous polyps during the same visit helps prevent cancer. For people with rectal bleeding, iron-deficiency anemia, a positive stool test, chronic diarrhea, or a strong family history, a prompt colonoscopy clarifies the cause and guides treatment. In short, the colonoscope lets your doctor diagnose and treat in one session.
Rectal bleeding, ongoing belly pain, changes in bowel habits, unexplained weight loss
Positive FIT or stool DNA test that needs confirmation by colonoscopy
Iron-deficiency anemia or long-lasting diarrhea without a clear cause
Removes adenomas to block the “polyp → cancer” pathway
Targets biopsies so diagnosis is faster and more accurate
Treats issues during the same visit (bleeding control, dilation, tattooing)
| Scenario | Colonoscopic goal | Typical outcome |
|---|---|---|
| Average-risk screening | Find/remove polyps | Return in years if normal |
| Positive stool test | Find the source | Biopsy or polyp removal |
| Symptoms present | Explain cause | Treatment plan and follow-up |
Most average-risk adults should start screening at the guideline-recommended age because the chance of advanced polyps rises with age. If a first-degree relative had colorectal cancer or an advanced adenoma, screening often starts earlier—sometimes 10 years before the relative’s diagnosis age. People with hereditary syndromes or long-standing inflammatory bowel disease need a customized plan that starts younger and repeats more often. Share your family history so your schedule can be tailored to you.
Begin at the recommended age for your country or region
If the exam is normal and high-quality, follow the standard interval
Support prevention with healthy habits (fiber, activity, no smoking)
Family history: begin earlier than average
Genetic syndromes (e.g., Lynch): start much earlier, repeat more often
Ulcerative colitis/Crohn’s colitis: start surveillance after years of disease
Several relatives with colorectal cancer or very young diagnoses
Personal history of adenomas or serrated lesions
Ongoing bleeding or anemia despite noninvasive tests
| Risk group | Typical start | Notes |
|---|---|---|
| Average risk | Guideline age | Longer interval if normal exam |
| One first-degree relative | Earlier start | Tighter follow-up |
| Hereditary syndromes | Very early | Specialist surveillance |
Frequency balances protection and practicality. If a normal, high-quality exam shows no polyps, the next check is usually years away. If polyps are found, the interval shortens based on how many, how big, and what type they are; advanced features mean closer follow-up. Inflammatory bowel disease, strong family history, or poor preparation can also shorten timelines. Your next due date always depends on today’s results—keep your report and share it at follow-ups.
Normal, high-quality exam: longest interval
One or two small low-risk adenomas: moderate interval
Three or more adenomas, large size, or advanced features: shortest interval
Incomplete exam or poor bowel prep → repeat sooner
Strong family history or genetic syndrome → closer surveillance
New “alarm” symptoms → evaluate promptly; do not wait
| Finding | Next interval | Comment |
|---|---|---|
| Normal, high-quality | Longest | Resume routine screening |
| Low-risk adenomas | Moderate | Ensure better prep next time |
| Advanced adenoma | Shortest | Expert surveillance recommended |
You check in, review medications and allergies, and receive a sedative through an IV for comfort. The doctor gently advances a flexible colonoscope to the beginning of the colon (cecum). Air or CO₂ opens the colon so the lining can be seen clearly; high-definition video highlights small, flat lesions. Polyps can be removed with a snare or forceps, and bleeding can be treated. After a slow, careful withdrawal and documentation, you rest briefly and go home the same day with a written report.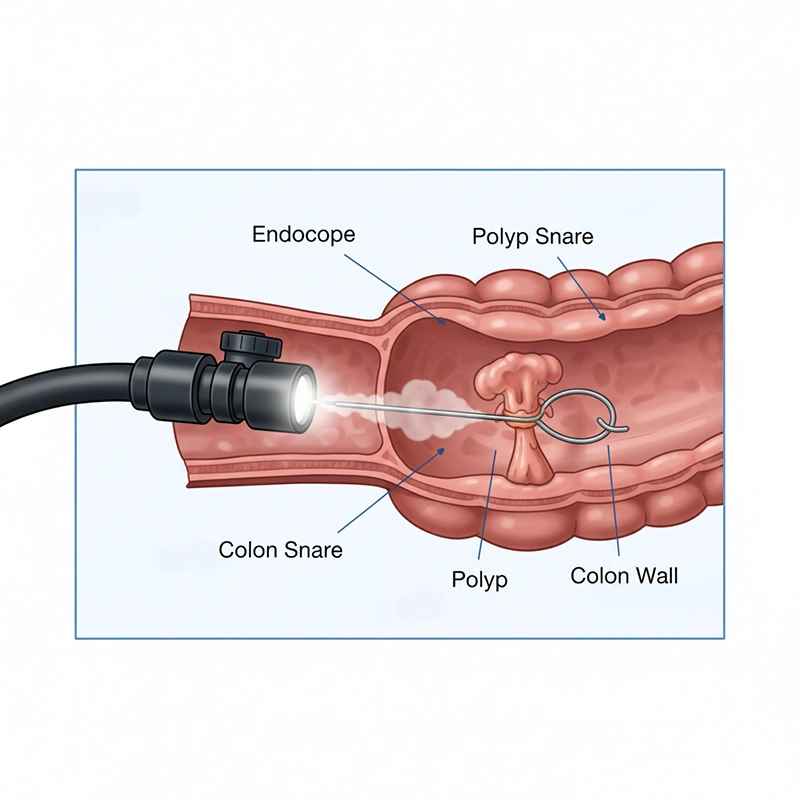
Arrival: consent, safety checks, vital signs
Sedation: continuous monitoring for comfort and safety
Exam: careful inspection during withdrawal to find subtle polyps
Aftercare: short recovery, light meal once fully awake
Photo confirmation of cecal intubation (full exam)
Adequate bowel preparation score for clear views
Sufficient withdrawal time to boost detection rates
| Step | Purpose | Outcome |
|---|---|---|
| Bowel prep review | Clear view | Fewer missed lesions |
| Reach the cecum | Complete exam | Whole-colon assessment |
| Slow withdrawal | Detection | Higher adenoma detection |
Colonoscopy is very safe, but minor effects like gas, bloating, or drowsiness are common and short-lived. Uncommon risks include bleeding—usually after polyp removal—and, rarely, a perforation (a tear in the bowel). Choosing an experienced endoscopist at a certified center lowers these risks. Sharing your full medication list (especially blood thinners) and following prep instructions closely further improves safety. If anything feels off afterward, call your care team quickly.
Gas, fullness, mild cramps from air or CO₂ used during the exam
Temporary sleepiness from sedation
Small blood streaks if tiny polyps were removed
Perforation that may need urgent care
Delayed bleeding after polyp removal
Reactions to sedatives or dehydration
Perforation: roughly 0.02%–0.1% for diagnostic exams; up to ~0.1%–0.3% with polyp removal
Clinically significant post-polypectomy bleeding: about 0.3%–1.0%; minor spotting can occur and usually settles
Sedation-related problems requiring intervention: uncommon, around 0.1%–0.5%; mild drowsiness is expected
Minor symptoms (bloating, cramps): common and short-lived in a noticeable fraction of patients
| Issue | Approx. frequency | What helps |
|---|---|---|
| Bloating/mild pain | Common, short-lived | Walk, hydrate, warm fluids |
| Bleeding needing care | ~0.3%–1.0% (after polypectomy) | Careful technique; call if persistent |
| Perforation | ~0.02%–0.1% diagnostic; higher with therapy | Experienced operator; prompt check-up |
Plan a ride home because of sedation. Start with light meals and plenty of fluids; most gas and cramps fade within hours. Read your printed report—it lists polyp size, number, and location—and expect pathology results in a few days if biopsies were taken. Call sooner for heavy bleeding, fever, severe abdominal pain, or repeated vomiting. Save all reports; your next colonoscopy date depends on today’s findings and the quality of the exam.
0–2 hours: rest in recovery; mild gas or sleepiness is common; start sipping fluids when cleared
Same day: light meals as tolerated; avoid driving, alcohol, and big decisions; walking eases bloating
24–48 hours: most people feel normal; minor spotting can occur after polyp removal; resume usual routine unless told otherwise
Don’t drive or sign legal papers after sedation
Eat lightly at first; increase as tolerated
Avoid alcohol for 24 hours and rehydrate well
Heavy or ongoing bleeding
Fever or worsening abdominal pain
Dizziness or inability to keep fluids down
| Symptom | Typical course | Action |
|---|---|---|
| Mild gas/bloating | Hours | Walk, warm drinks |
| Small blood streaks | 24–48 hours | Watch; call if increasing |
| Severe pain/fever | Not expected | Seek urgent care |
Colonoscopy is the gold standard because it can both find and remove precancerous lesions in one visit. A single high-quality exam lowers future cancer risk by clearing adenomas that might otherwise grow over years. Screening programs with good participation improve survival across whole communities. Noninvasive tests are helpful, but a positive result still needs a colonoscopic exam. Following a clear, guideline-based schedule with a skilled team gives the best long-term protection.
Direct view of the bowel lining with a colonoscope
Immediate removal of suspicious polyps
Biopsies for precise answers when needed
Public awareness and easy access to screening
High-quality bowel prep and complete exams
Reliable follow-up after positive noninvasive tests
| Feature | Colonoscopy benefit |
|---|---|
| Detect + treat | Removes lesions immediately |
| Full-length view | Checks the entire colon and rectum |
| Histology | Biopsy confirms diagnosis |
Good preparation is the single most important part of the test. A clean colon lets the doctor see small, flat lesions and avoids repeat exams. Follow a low-residue diet as advised, then switch to clear liquids the day before. Take the split-dose laxative exactly on schedule; finish the second half several hours before arrival. If you see “colonoscop prep” mentioned online, it simply means colonoscopy preparation steps. Work with your clinician to adjust blood thinners and diabetes medicines safely. Great prep makes the colonoscopy shorter, safer, and more accurate.
Low-residue diet 2–3 days prior if advised
Clear liquids the day before; avoid red or blue dyes
Nothing by mouth during the fasting window your team sets
Split-dose prep cleans better than a single dose
Chill the solution and use a straw to make it easier
Keep sipping clear liquids until the cutoff time
Case 1 (mistake): stopped clear liquids early and rushed the first dose → Result: thick output on exam morning; poor visibility. Correction: finish the first dose on time, keep clear liquids up to the allowed cutoff, and start dose two at the scheduled hour.
Case 2 (mistake): ate high-fiber food the afternoon before prep → Result: residual solids; exam had to be rescheduled. Correction: begin low-residue earlier and avoid seeds, skins, whole grains for 2–3 days if advised.
Case 3 (mistake): took blood thinner without checking → Result: procedure delayed for safety. Correction: review all medicines with the team a week ahead; follow the exact pause/bridge plan.
| Problem | Likely cause | Fix |
|---|---|---|
| Brown liquid output | Incomplete prep | Finish dose; extend clear liquids |
| Nausea | Drinking too fast | Sip steadily; brief pauses |
| Residual solids | Too much fiber close to exam | Start low-residue earlier next time |
Myths can keep people from helpful care. Clearing them up makes decisions easier and safer for everyone considering a colonoscopy.
| Myth | Fact | Why it matters |
|---|---|---|
| Colonoscopy always hurts. | Sedation keeps most people comfortable. | Comfort improves completion and quality. |
| You can’t eat for days. | Clear liquids the day before; normal eating resumes soon after. | Realistic prep lowers anxiety and drop-offs. |
| Polyps mean cancer. | Most polyps are benign; removal prevents cancer. | Prevention is the goal, not fear. |
| A positive stool test replaces colonoscopy. | A positive test requires a colonoscopic exam. | Only colonoscopy can confirm and treat. |
| Only older adults need screening. | Start at guideline age; earlier if high-risk. | Early detection saves lives. |
| Prep is dangerous. | Prep is generally safe; hydration and timing help. | Good prep improves safety and accuracy. |
| One colonoscopy lasts for life. | Intervals depend on findings and risk. | Follow the schedule your report sets. |
| Bleeding for a week is normal. | Minor streaks may occur; persistent bleeding needs a call. | Early reporting prevents complications. |
With careful preparation and an experienced team, colonoscopy using a modern colonoscope offers a safe, effective way to prevent cancer and explain troubling symptoms. Normal results usually mean a long interval until the next test, while polyps or higher-risk findings call for closer follow-up. Keep your reports, update family history, and follow the plan you agree on. With a clear colonoscop-informed schedule and timely colonoscopic care, most people maintain strong, long-term protection against colorectal cancer.
A colonoscopy is a test of the large intestine that uses a flexible video colonoscope to show the inner lining on a screen. The doctor can remove polyps and take biopsies in the same visit.
Most average risk adults start at the guideline age for screening. If a close relative had colorectal cancer or an advanced adenoma you may start earlier by about ten years before the relatives diagnosis age.
After a high quality normal exam the next check is set for a long interval. Your report lists the due date and you should bring that report to future visits.
A colonoscopic exam lets the doctor see the whole colon and remove precancerous lesions right away. This lowers future cancer risk more than tests that only detect blood or DNA in stool.
Rectal bleeding persistent bowel change iron deficiency anemia positive stool test and unexplained abdominal pain are common triggers. A strong family history also supports timely evaluation.
Copyright © 2025.Geekvalue All rights reserved.Technical Support:TiaoQingCMS