ಪರಿವಿಡಿ
ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಎನ್ನುವುದು ಕನಿಷ್ಠ ಆಕ್ರಮಣಕಾರಿ ಸ್ತ್ರೀರೋಗ ಶಾಸ್ತ್ರದ ವಿಧಾನವಾಗಿದ್ದು, ವೈದ್ಯರು ಹಿಸ್ಟರೊಸ್ಕೋಪ್ ಎಂಬ ವಿಶೇಷ ಉಪಕರಣವನ್ನು ಬಳಸಿಕೊಂಡು ಗರ್ಭಾಶಯದ ಒಳಭಾಗವನ್ನು ನೋಡಲು ಅನುವು ಮಾಡಿಕೊಡುತ್ತದೆ. ಇದನ್ನು ರೋಗನಿರ್ಣಯ ಮತ್ತು ಶಸ್ತ್ರಚಿಕಿತ್ಸಾ ಹಿಸ್ಟರೊಸ್ಕೋಪಿಗೆ ಬಳಸಲಾಗುತ್ತದೆ, ಅಸಹಜ ರಕ್ತಸ್ರಾವ, ಫೈಬ್ರಾಯ್ಡ್ಗಳು, ಅಂಟಿಕೊಳ್ಳುವಿಕೆಗಳು ಮತ್ತು ಪಾಲಿಪ್ಸ್ನಂತಹ ಗರ್ಭಾಶಯದ ಸ್ಥಿತಿಗಳಿಗೆ ಚಿಕಿತ್ಸೆ ನೀಡಲು, ಹೊಟ್ಟೆಯ ಛೇದನವಿಲ್ಲದೆ ಮತ್ತು ಸಾಮಾನ್ಯವಾಗಿ ವೇಗವಾಗಿ ಚೇತರಿಸಿಕೊಳ್ಳದೆ.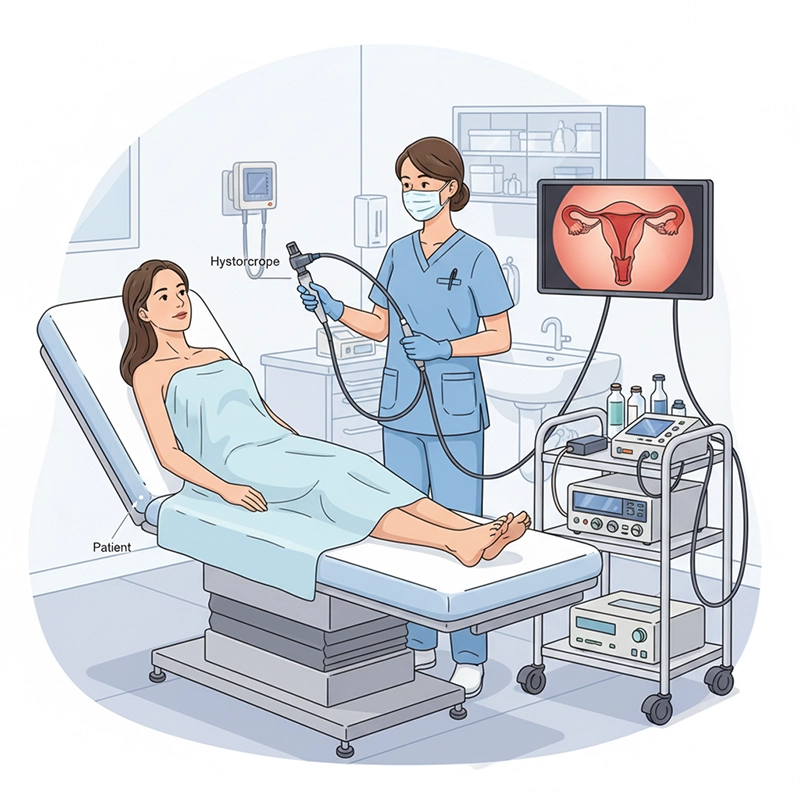
ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಎನ್ನುವುದು ಗರ್ಭಕಂಠದ ಮೂಲಕ ಹಿಸ್ಟರೊಸ್ಕೋಪ್ ಅನ್ನು ಸೇರಿಸುವ ಮೂಲಕ ಗರ್ಭಾಶಯದ ಕುಹರದ ಎಂಡೋಸ್ಕೋಪಿಕ್ ಪರೀಕ್ಷೆಯಾಗಿದೆ. ಇದು ಅಲ್ಟ್ರಾಸೌಂಡ್ ಅಥವಾ ಎಂಆರ್ಐನಿಂದ ಸಂಪೂರ್ಣವಾಗಿ ನಿರೂಪಿಸಲ್ಪಡದ ಗರ್ಭಾಶಯದ ಅಸಹಜತೆಗಳನ್ನು ಗುರುತಿಸಲು ಮತ್ತು ಅಗತ್ಯವಿದ್ದಾಗ ಚಿಕಿತ್ಸೆ ನೀಡಲು ಎಂಡೊಮೆಟ್ರಿಯಂನ ನೇರ ದೃಶ್ಯೀಕರಣವನ್ನು ಶಕ್ತಗೊಳಿಸುತ್ತದೆ.
ರೋಗನಿರ್ಣಯದ ಹಿಸ್ಟರೊಸ್ಕೋಪಿ: ಅಸಹಜ ಗರ್ಭಾಶಯದ ರಕ್ತಸ್ರಾವ, ಬಂಜೆತನ ಅಥವಾ ಶಂಕಿತ ರೋಗಶಾಸ್ತ್ರವನ್ನು ತನಿಖೆ ಮಾಡಲು ದೃಶ್ಯ ಮೌಲ್ಯಮಾಪನ.
ಶಸ್ತ್ರಚಿಕಿತ್ಸಾ ಹಿಸ್ಟರೋಸ್ಕೋಪಿ (ಆಪರೇಟಿವ್ ಹಿಸ್ಟರೋಸ್ಕೋಪಿ): ಪಾಲಿಪ್ಸ್, ಫೈಬ್ರಾಯ್ಡ್ಗಳು ಅಥವಾ ಅಂಟಿಕೊಳ್ಳುವಿಕೆಯನ್ನು ತೆಗೆದುಹಾಕಲು ಅಥವಾ ಗರ್ಭಾಶಯದ ಸೆಪ್ಟಮ್ ಅನ್ನು ಸರಿಪಡಿಸಲು ಚಿಕಣಿ ಉಪಕರಣಗಳನ್ನು ಬಳಸಿಕೊಂಡು ದೃಶ್ಯೀಕರಣ ಮತ್ತು ಚಿಕಿತ್ಸೆ.
ಈ ವಿಧಾನವು ಟ್ರಾನ್ಸ್-ಸರ್ವಿಕಲ್ ಆಗಿರುವುದರಿಂದ, ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಹೊಟ್ಟೆಯ ಛೇದನವನ್ನು ತಪ್ಪಿಸುತ್ತದೆ, ಚೇತರಿಕೆಯ ಸಮಯವನ್ನು ಕಡಿಮೆ ಮಾಡುತ್ತದೆ ಮತ್ತು ಮುಕ್ತ ಕಾರ್ಯವಿಧಾನಗಳಿಗೆ ಹೋಲಿಸಿದರೆ ಫಲವತ್ತತೆಯ ಸಾಮರ್ಥ್ಯವನ್ನು ಸಂರಕ್ಷಿಸುತ್ತದೆ.
ಹಿಸ್ಟರೊಸ್ಕೋಪ್ ಎನ್ನುವುದು ತೆಳುವಾದ, ಟ್ಯೂಬ್ ತರಹದ ಸಾಧನವಾಗಿದ್ದು, ಇದರಲ್ಲಿ ಆಪ್ಟಿಕಲ್ ಅಥವಾ ಡಿಜಿಟಲ್ ಕ್ಯಾಮೆರಾ ಮತ್ತು ಬೆಳಕಿನ ಮೂಲವಿದೆ, ಇದು ನೈಜ-ಸಮಯದ ಮಾರ್ಗದರ್ಶನಕ್ಕಾಗಿ ಚಿತ್ರಗಳನ್ನು ಮಾನಿಟರ್ಗೆ ರವಾನಿಸುತ್ತದೆ.
ನೇರ ದೃಶ್ಯೀಕರಣಕ್ಕಾಗಿ ಆಪ್ಟಿಕಲ್ ಲೆನ್ಸ್ ಅಥವಾ ಡಿಜಿಟಲ್ ಕ್ಯಾಮೆರಾ
ಪ್ರಕಾಶಕ್ಕಾಗಿ ಹೆಚ್ಚಿನ ತೀವ್ರತೆಯ ಬೆಳಕಿನ ಮೂಲ
ವಾದ್ಯಗಳಿಗೆ ಕೆಲಸ ಮಾಡುವ ಚಾನಲ್ಗಳು (ಕತ್ತರಿ, ಗ್ರಾಸ್ಪರ್ಗಳು, ಮೊರ್ಸೆಲೇಟರ್ಗಳು)
ಗರ್ಭಾಶಯದ ಕುಹರವನ್ನು ವಿಸ್ತರಿಸಲು CO₂ ಅಥವಾ ಸಲೈನ್ ಬಳಸುವ ವಿಸ್ತರಣಾ ವ್ಯವಸ್ಥೆ.
ರಿಜಿಡ್ ಹಿಸ್ಟರೊಸ್ಕೋಪ್ಗಳು: ಹೈ-ಡೆಫಿನಿಷನ್ ಇಮೇಜಿಂಗ್; ಸಾಮಾನ್ಯವಾಗಿ ಶಸ್ತ್ರಚಿಕಿತ್ಸಾ/ಶಸ್ತ್ರಚಿಕಿತ್ಸಾ ಹಿಸ್ಟರೊಸ್ಕೋಪಿಗೆ ಬಳಸಲಾಗುತ್ತದೆ.
ಹೊಂದಿಕೊಳ್ಳುವ ಹಿಸ್ಟರೊಸ್ಕೋಪ್ಗಳು: ಹೆಚ್ಚಿನ ಆರಾಮ; ಸಾಮಾನ್ಯವಾಗಿ ರೋಗನಿರ್ಣಯದ ಹಿಸ್ಟರೊಸ್ಕೋಪಿಗೆ.
ಮಿನಿ-ಹಿಸ್ಟರೊಸ್ಕೋಪ್ಗಳು: ಕನಿಷ್ಠ ಅರಿವಳಿಕೆಯೊಂದಿಗೆ ಕಚೇರಿ ಆಧಾರಿತ ಕಾರ್ಯವಿಧಾನಗಳಿಗೆ ಸೂಕ್ತವಾದ ಸಣ್ಣ ವ್ಯಾಸದ ಸ್ಕೋಪ್ಗಳು.
ಅಸಹಜ ಗರ್ಭಾಶಯ ರಕ್ತಸ್ರಾವ (AUB): ಭಾರೀ ಅಥವಾ ಅನಿಯಮಿತ ರಕ್ತಸ್ರಾವದ ಮೌಲ್ಯಮಾಪನ; ಪಾಲಿಪ್ಸ್, ಫೈಬ್ರಾಯ್ಡ್ಗಳು ಅಥವಾ ಹೈಪರ್ಪ್ಲಾಸಿಯಾ ಪತ್ತೆ.
ಬಂಜೆತನದ ಮೌಲ್ಯಮಾಪನಗಳು: ಗರ್ಭಧಾರಣೆಯನ್ನು ತಡೆಯುವ ಪಾಲಿಪ್ಸ್, ಅಂಟಿಕೊಳ್ಳುವಿಕೆಗಳು ಅಥವಾ ಸೆಪ್ಟಾಗಳ ಗುರುತಿಸುವಿಕೆ.
ಪುನರಾವರ್ತಿತ ಗರ್ಭ ನಷ್ಟ: ಜನ್ಮಜಾತ ವೈಪರೀತ್ಯಗಳು ಅಥವಾ ಗುರುತುಗಳ ಪತ್ತೆ.
ಗರ್ಭಾಶಯದ ಫೈಬ್ರಾಯ್ಡ್ಗಳು ಮತ್ತು ಎಂಡೊಮೆಟ್ರಿಯಲ್ ಪಾಲಿಪ್ಸ್: ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಪಾಲಿಪೆಕ್ಟಮಿ ಅಥವಾ ಮೈಯೊಮೆಕ್ಟಮಿಗೆ ಯೋಜನೆ.
ಗರ್ಭಾಶಯದೊಳಗೆ ಅಂಟಿಕೊಳ್ಳುವಿಕೆಗಳು (ಆಶರ್ಮನ್ ಸಿಂಡ್ರೋಮ್): ಕುಹರವನ್ನು ಪುನಃಸ್ಥಾಪಿಸಲು ಹಿಸ್ಟರೊಸ್ಕೋಪಿಕ್ ಅಥೆಸಿಯೊಲಿಸಿಸ್.
ವಿದೇಶಿ ದೇಹ ತೆಗೆಯುವಿಕೆ: ಉಳಿಸಿಕೊಂಡಿರುವ ಐಯುಡಿಗಳು ಅಥವಾ ಇತರ ಗರ್ಭಾಶಯದ ಒಳಗಿನ ವಸ್ತುಗಳ ಮಾರ್ಗದರ್ಶಿ ಮರುಪಡೆಯುವಿಕೆ.
ರೋಗನಿರ್ಣಯ ಮತ್ತು ಶಸ್ತ್ರಚಿಕಿತ್ಸೆಯ ಪ್ರಕರಣಗಳಿಗೆ ಅನುಕ್ರಮವು ಸ್ವಲ್ಪ ಭಿನ್ನವಾಗಿರುತ್ತದೆ, ಆದರೆ ಸುರಕ್ಷತೆ ಮತ್ತು ನಿಖರತೆಯನ್ನು ಕಾಪಾಡಿಕೊಳ್ಳಲು ಪ್ರಮುಖ ಹಂತಗಳು ಸ್ಥಿರವಾಗಿರುತ್ತವೆ.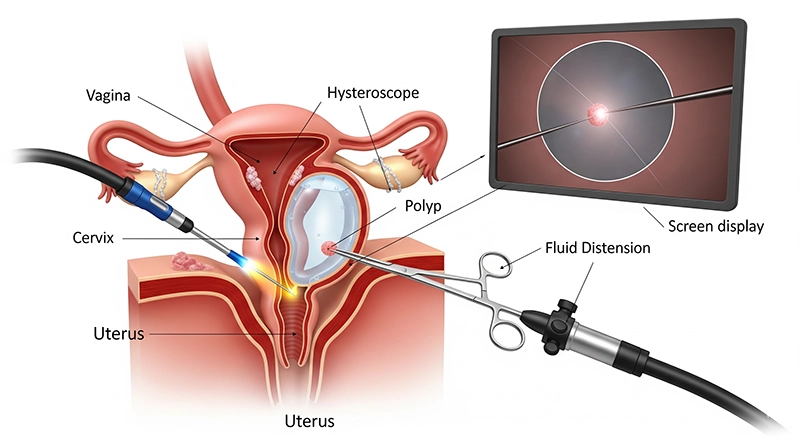
ಇತಿಹಾಸ ಮತ್ತು ಪರೀಕ್ಷೆ: ಮುಟ್ಟಿನ ಮಾದರಿ, ಹಿಂದಿನ ಶಸ್ತ್ರಚಿಕಿತ್ಸೆಗಳು, ಅಪಾಯಕಾರಿ ಅಂಶಗಳು
ಇಮೇಜಿಂಗ್: ಸೂಚಿಸಿದಾಗ ಅಲ್ಟ್ರಾಸೌಂಡ್ ಅಥವಾ ಎಂಆರ್ಐ
ತಿಳುವಳಿಕೆಯುಳ್ಳ ಒಪ್ಪಿಗೆ ಮತ್ತು ಪರ್ಯಾಯಗಳ ಚರ್ಚೆ
ರೋಗನಿರ್ಣಯದ ಹಿಸ್ಟರೊಸ್ಕೋಪಿ: ಸಾಮಾನ್ಯವಾಗಿ ಕಡಿಮೆ ಅಥವಾ ಅರಿವಳಿಕೆ ಇಲ್ಲದೆ ಕಚೇರಿ ಆಧಾರಿತ.
ಆಪರೇಟಿವ್ ಹಿಸ್ಟರೊಸ್ಕೋಪಿ: ಸಂಕೀರ್ಣತೆಯನ್ನು ಅವಲಂಬಿಸಿ ಸ್ಥಳೀಯ, ಪ್ರಾದೇಶಿಕ ಅಥವಾ ಸಾಮಾನ್ಯ ಅರಿವಳಿಕೆ.
ಅಗತ್ಯವಿರುವಂತೆ ಗರ್ಭಕಂಠದ ತಯಾರಿ ಅಥವಾ ಹಿಗ್ಗುವಿಕೆ
ಗರ್ಭಾಶಯದ ಕುಹರವನ್ನು ಹಿಗ್ಗಿಸಲು CO₂ ಅಥವಾ ಲವಣಯುಕ್ತ ದ್ರಾವಣವನ್ನು ಪರಿಚಯಿಸುವುದು.
ಗರ್ಭಕಂಠದ ಮೂಲಕ ಹಿಸ್ಟರೊಸ್ಕೋಪ್ ಅನ್ನು ಎಚ್ಚರಿಕೆಯಿಂದ ಸೇರಿಸುವುದು.
ಮಾನಿಟರ್ನಲ್ಲಿ ಎಂಡೊಮೆಟ್ರಿಯಲ್ ಕುಹರದ ವ್ಯವಸ್ಥಿತ ದೃಶ್ಯೀಕರಣ
ವ್ಯಾಪ್ತಿಯ ಮೂಲಕ ರವಾನಿಸಲಾದ ಉಪಕರಣಗಳನ್ನು ಬಳಸಿಕೊಂಡು ಗುರುತಿಸಲಾದ ರೋಗಶಾಸ್ತ್ರದ ಚಿಕಿತ್ಸೆ.
ಹಿಸ್ಟರೊಸ್ಕೋಪಿಯನ್ನು ಡಿಲೇಷನ್ ಮತ್ತು ಕ್ಯುರೆಟ್ಟೇಜ್ (ಡಿ&ಸಿ) ನೊಂದಿಗೆ ಸಂಯೋಜಿಸಿದಾಗ, ಅದನ್ನು ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಡಿ&ಸಿ ಎಂದು ಕರೆಯಲಾಗುತ್ತದೆ. ಗರ್ಭಕಂಠವನ್ನು ಹಿಗ್ಗಿಸಲಾಗುತ್ತದೆ ಮತ್ತು ಎಂಡೊಮೆಟ್ರಿಯಲ್ ಅಂಗಾಂಶವನ್ನು ನೇರ ದೃಶ್ಯೀಕರಣದ ಅಡಿಯಲ್ಲಿ ತೆಗೆದುಹಾಕಲಾಗುತ್ತದೆ, ಇದು ಬ್ಲೈಂಡ್ ಕ್ಯುರೆಟ್ಟೇಜ್ಗೆ ಹೋಲಿಸಿದರೆ ನಿಖರತೆಯನ್ನು ಸುಧಾರಿಸುತ್ತದೆ.
ಒಂದೇ ಅವಧಿಯಲ್ಲಿ ಎಂಡೊಮೆಟ್ರಿಯಲ್ ಪಾಲಿಪ್ಗಳನ್ನು ತೆಗೆದುಹಾಕಿದರೆ, ಆ ವಿಧಾನವನ್ನು ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಡಿ & ಸಿ ಪಾಲಿಪೆಕ್ಟಮಿ ಎಂದು ಕರೆಯಲಾಗುತ್ತದೆ. ಈ ವಿಧಾನವು ಒಂದೇ ಭೇಟಿಯಲ್ಲಿ ಗುರಿ ಮಾದರಿ ಮತ್ತು ಚಿಕಿತ್ಸೆಯನ್ನು ಸಕ್ರಿಯಗೊಳಿಸುತ್ತದೆ.
ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಒಂದೇ ತಂತ್ರವಲ್ಲ, ಬದಲಾಗಿ ಹಲವಾರು ಉದ್ದೇಶಿತ ಕಾರ್ಯವಿಧಾನಗಳನ್ನು ಸಕ್ರಿಯಗೊಳಿಸುವ ವೇದಿಕೆಯಾಗಿದೆ. ರೋಗಿಯ ಸ್ಥಿತಿಯನ್ನು ಅವಲಂಬಿಸಿ, ವೈದ್ಯರು ವ್ಯಾಪಕ ಶ್ರೇಣಿಯ ಹಿಸ್ಟರೊಸ್ಕೋಪಿಕ್ ಚಿಕಿತ್ಸೆಗಳಿಂದ ಆಯ್ಕೆ ಮಾಡಬಹುದು. ಸಾಮಾನ್ಯವಾದವುಗಳು:
ಈ ವಿಧಾನವು ಹಿಸ್ಟರೊಸ್ಕೋಪಿಕ್ ದೃಶ್ಯೀಕರಣವನ್ನು ಹಿಗ್ಗುವಿಕೆ ಮತ್ತು ಕ್ಯುರೆಟ್ಟೇಜ್ನೊಂದಿಗೆ ಸಂಯೋಜಿಸುತ್ತದೆ. ಅಸಹಜ ಗರ್ಭಾಶಯದ ರಕ್ತಸ್ರಾವವನ್ನು ಅನುಭವಿಸುತ್ತಿರುವ ಮಹಿಳೆಯರಿಗೆ ಅಥವಾ ಮಾರಕತೆಯನ್ನು ತಳ್ಳಿಹಾಕಲು ಅಂಗಾಂಶ ಮಾದರಿ ಅಗತ್ಯವಿದ್ದಾಗ ಇದನ್ನು ಹೆಚ್ಚಾಗಿ ನಡೆಸಲಾಗುತ್ತದೆ. ಹಿಸ್ಟರೊಸ್ಕೋಪ್ ಒದಗಿಸಿದ ಮಾರ್ಗದರ್ಶನವು ಈ ವಿಧಾನವನ್ನು ಸಾಂಪ್ರದಾಯಿಕ ಬ್ಲೈಂಡ್ ಕ್ಯುರೆಟ್ಟೇಜ್ಗಿಂತ ಸುರಕ್ಷಿತ ಮತ್ತು ಹೆಚ್ಚು ನಿಖರವಾಗಿ ಮಾಡುತ್ತದೆ.
ಎಂಡೊಮೆಟ್ರಿಯಲ್ ಪಾಲಿಪ್ಸ್ ಗರ್ಭಾಶಯದ ಒಳಪದರದ ಹಾನಿಕರವಲ್ಲದ ಬೆಳವಣಿಗೆಗಳಾಗಿದ್ದು, ಇದು ಭಾರೀ ರಕ್ತಸ್ರಾವ ಅಥವಾ ಬಂಜೆತನಕ್ಕೆ ಕಾರಣವಾಗಬಹುದು. ಹಿಸ್ಟರೊಸ್ಕೋಪಿಕ್ ಪಾಲಿಪೆಕ್ಟಮಿಯು ಪಾಲಿಪ್ ಅನ್ನು ನೇರವಾಗಿ ದೃಶ್ಯೀಕರಿಸುವುದು ಮತ್ತು ಶಸ್ತ್ರಚಿಕಿತ್ಸಾ ಕತ್ತರಿ, ಎಲೆಕ್ಟ್ರೋಸರ್ಜಿಕಲ್ ಲೂಪ್ಗಳು ಅಥವಾ ಟಿಶ್ಯೂ ಮಾರ್ಸಲೇಟರ್ಗಳನ್ನು ಬಳಸಿ ಅದನ್ನು ತೆಗೆದುಹಾಕುವುದನ್ನು ಒಳಗೊಂಡಿರುತ್ತದೆ. ಕಾರ್ಯವಿಧಾನವು ಕನಿಷ್ಠ ಆಕ್ರಮಣಕಾರಿಯಾಗಿರುವುದರಿಂದ, ಹೆಚ್ಚಿನ ರೋಗಿಗಳು ಬೇಗನೆ ಚೇತರಿಸಿಕೊಳ್ಳುತ್ತಾರೆ ಮತ್ತು ರೋಗಲಕ್ಷಣಗಳಲ್ಲಿ ತಕ್ಷಣದ ಸುಧಾರಣೆಯನ್ನು ಅನುಭವಿಸುತ್ತಾರೆ.
ಕೆಲವು ಸಂದರ್ಭಗಳಲ್ಲಿ, ಅಂಗಾಂಶ ಮಾದರಿ ಸಂಗ್ರಹಣೆ ಮತ್ತು ಪಾಲಿಪ್ ತೆಗೆಯುವಿಕೆ ಎರಡನ್ನೂ ಒಟ್ಟಿಗೆ ನಡೆಸಲಾಗುತ್ತದೆ. ಈ ಸಂಯೋಜಿತ ವಿಧಾನವು ಆಧಾರವಾಗಿರುವ ರೋಗಶಾಸ್ತ್ರಕ್ಕೆ ಚಿಕಿತ್ಸೆ ನೀಡುವಾಗ ಗರ್ಭಾಶಯದ ಕುಹರದ ಸಮಗ್ರ ಮೌಲ್ಯಮಾಪನವನ್ನು ಖಚಿತಪಡಿಸುತ್ತದೆ.
ಸಬ್ಮ್ಯೂಕೋಸಲ್ ಫೈಬ್ರಾಯ್ಡ್ಗಳು ಗರ್ಭಾಶಯದ ಕುಹರದೊಳಗೆ ಚಾಚಿಕೊಂಡಿರುವ ಕ್ಯಾನ್ಸರ್ ರಹಿತ ಬೆಳವಣಿಗೆಗಳಾಗಿವೆ. ಹಿಸ್ಟರೊಸ್ಕೋಪಿಕ್ ಮೈಯೊಮೆಕ್ಟಮಿಯು ಹೊಟ್ಟೆಯ ಛೇದನವಿಲ್ಲದೆ ಅವುಗಳನ್ನು ತೆಗೆದುಹಾಕಲು ಅನುವು ಮಾಡಿಕೊಡುತ್ತದೆ. ಫೈಬ್ರಾಯ್ಡ್ ಅಂಗಾಂಶವನ್ನು ಕ್ಷೌರ ಮಾಡಲು ಅಥವಾ ಕತ್ತರಿಸಲು ವಿಶೇಷ ರೆಸೆಕ್ಟೋಸ್ಕೋಪ್ಗಳು ಅಥವಾ ಮಾರ್ಸಲೇಟರ್ಗಳನ್ನು ಬಳಸಲಾಗುತ್ತದೆ, ಗರ್ಭಾಶಯವನ್ನು ಸಂರಕ್ಷಿಸುತ್ತದೆ ಮತ್ತು ಫಲವತ್ತತೆಯ ಸಾಮರ್ಥ್ಯವನ್ನು ಕಾಪಾಡಿಕೊಳ್ಳುತ್ತದೆ.
ಗರ್ಭಾಶಯದ ಸೆಪ್ಟಮ್ ಒಂದು ಜನ್ಮಜಾತ ಅಸಂಗತತೆಯಾಗಿದ್ದು, ಇದರಲ್ಲಿ ನಾರಿನ ಗೋಡೆಯು ಗರ್ಭಾಶಯದ ಕುಹರವನ್ನು ವಿಭಜಿಸುತ್ತದೆ, ಇದು ಹೆಚ್ಚಾಗಿ ಬಂಜೆತನ ಮತ್ತು ಮರುಕಳಿಸುವ ಗರ್ಭಪಾತಕ್ಕೆ ಸಂಬಂಧಿಸಿದೆ. ಹಿಸ್ಟರೊಸ್ಕೋಪಿಕ್ ಸೆಪ್ಟಮ್ ರಿಸೆಕ್ಷನ್ ನೇರ ದೃಶ್ಯೀಕರಣದ ಅಡಿಯಲ್ಲಿ ಸೆಪ್ಟಮ್ ಅನ್ನು ಕತ್ತರಿಸುವುದು, ಸಾಮಾನ್ಯ ಕುಹರದ ಆಕಾರವನ್ನು ಪುನಃಸ್ಥಾಪಿಸುವುದು ಮತ್ತು ಗರ್ಭಧಾರಣೆಯ ಫಲಿತಾಂಶಗಳನ್ನು ಸುಧಾರಿಸುವುದನ್ನು ಒಳಗೊಂಡಿರುತ್ತದೆ.
ಆಶರ್ಮನ್ ಸಿಂಡ್ರೋಮ್ ಎಂದೂ ಕರೆಯಲ್ಪಡುವ ಗರ್ಭಾಶಯದೊಳಗೆ ಅಂಟಿಕೊಳ್ಳುವಿಕೆಗಳು ಸೋಂಕು ಅಥವಾ ಗರ್ಭಾಶಯದ ಶಸ್ತ್ರಚಿಕಿತ್ಸೆಯ ನಂತರ ರೂಪುಗೊಳ್ಳಬಹುದು. ಹಿಸ್ಟರೊಸ್ಕೋಪಿಕ್ ಅಡೆಸಿಯೋಲಿಸಿಸ್ ಗಾಯದ ಅಂಗಾಂಶವನ್ನು ಎಚ್ಚರಿಕೆಯಿಂದ ಬೇರ್ಪಡಿಸಲು, ಗರ್ಭಾಶಯದ ಕುಹರವನ್ನು ಪುನಃಸ್ಥಾಪಿಸಲು ಮತ್ತು ಮುಟ್ಟಿನ ಹರಿವು ಮತ್ತು ಫಲವತ್ತತೆಯನ್ನು ಸುಧಾರಿಸಲು ಸೂಕ್ಷ್ಮ ಕತ್ತರಿ ಅಥವಾ ಶಕ್ತಿ ಆಧಾರಿತ ಸಾಧನಗಳನ್ನು ಬಳಸುತ್ತದೆ.
ಭವಿಷ್ಯದಲ್ಲಿ ಫಲವತ್ತತೆಯನ್ನು ಬಯಸದ ಭಾರೀ ಮುಟ್ಟಿನ ರಕ್ತಸ್ರಾವ ಹೊಂದಿರುವ ಮಹಿಳೆಯರಿಗೆ, ಹಿಸ್ಟರೊಸ್ಕೋಪಿಕ್ ಎಂಡೊಮೆಟ್ರಿಯಲ್ ಅಬ್ಲೇಶನ್ ಗರ್ಭಾಶಯದ ಒಳಪದರವನ್ನು ನಾಶಪಡಿಸುತ್ತದೆ ಅಥವಾ ತೆಗೆದುಹಾಕುತ್ತದೆ. ಉಷ್ಣ ಶಕ್ತಿ, ರೇಡಿಯೋಫ್ರೀಕ್ವೆನ್ಸಿ ಮತ್ತು ಛೇದನ ಸೇರಿದಂತೆ ಹಲವಾರು ತಂತ್ರಗಳು ಲಭ್ಯವಿದೆ.
ತೆರೆದ ಶಸ್ತ್ರಚಿಕಿತ್ಸೆಗಿಂತ ಭಿನ್ನವಾಗಿ, ಹಿಸ್ಟರೊಸ್ಕೋಪಿಯು ಕಿಬ್ಬೊಟ್ಟೆಯ ಛೇದನವನ್ನು ತಪ್ಪಿಸುತ್ತದೆ. ಹಿಸ್ಟರೊಸ್ಕೋಪ್ ಗರ್ಭಕಂಠದ ಮೂಲಕ ಸ್ವಾಭಾವಿಕವಾಗಿ ಹಾದುಹೋಗುತ್ತದೆ, ಆಘಾತ ಮತ್ತು ವ್ಯಾಪಕ ಚೇತರಿಕೆಯ ಅಗತ್ಯವನ್ನು ಕಡಿಮೆ ಮಾಡುತ್ತದೆ.
ರೋಗನಿರ್ಣಯದ ಹಿಸ್ಟರೊಸ್ಕೋಪಿಗೆ ಒಳಗಾಗುವ ಹೆಚ್ಚಿನ ರೋಗಿಗಳು ಕೆಲವೇ ಗಂಟೆಗಳಲ್ಲಿ ಸಾಮಾನ್ಯ ಚಟುವಟಿಕೆಗಳಿಗೆ ಮರಳಬಹುದು. ಸಾಂಪ್ರದಾಯಿಕ ಶಸ್ತ್ರಚಿಕಿತ್ಸೆಗಳಿಗೆ ಹೋಲಿಸಿದರೆ ಶಸ್ತ್ರಚಿಕಿತ್ಸಾ ಹಿಸ್ಟರೊಸ್ಕೋಪಿಗೆ ಸಹ ಸಾಮಾನ್ಯವಾಗಿ ಸಂಕ್ಷಿಪ್ತ ಚೇತರಿಕೆಯ ಅವಧಿ ಬೇಕಾಗುತ್ತದೆ.
ದೊಡ್ಡ ಛೇದನಗಳಿಲ್ಲದೆ ಗರ್ಭಾಶಯವನ್ನು ಪ್ರವೇಶಿಸುವುದರಿಂದ, ಸೋಂಕು, ಗಾಯದ ಗುರುತು ಮತ್ತು ಶಸ್ತ್ರಚಿಕಿತ್ಸೆಯ ನಂತರದ ನೋವಿನ ಅಪಾಯ ಕಡಿಮೆ ಇರುತ್ತದೆ. ಆಸ್ಪತ್ರೆಯ ವಾಸ್ತವ್ಯವು ಹೆಚ್ಚಾಗಿ ಅನಗತ್ಯವಾಗಿರುತ್ತದೆ, ಇದು ಅಪಾಯಗಳು ಮತ್ತು ವೆಚ್ಚಗಳನ್ನು ಮತ್ತಷ್ಟು ಕಡಿಮೆ ಮಾಡುತ್ತದೆ.
ಶಸ್ತ್ರಚಿಕಿತ್ಸಾ ಹಿಸ್ಟರೊಸ್ಕೋಪಿಯ ಒಂದು ದೊಡ್ಡ ಪ್ರಯೋಜನವೆಂದರೆ ಗರ್ಭಾಶಯದ ಸಮಸ್ಯೆಗಳನ್ನು ಸರಿಪಡಿಸುವ ಸಾಮರ್ಥ್ಯ ಮತ್ತು ಫಲವತ್ತತೆಯ ಸಾಮರ್ಥ್ಯವನ್ನು ಸಂರಕ್ಷಿಸುವ ಅಥವಾ ಸುಧಾರಿಸುವ ಸಾಮರ್ಥ್ಯ. ಗರ್ಭಧಾರಣೆಯನ್ನು ಬಯಸುವ ಮಹಿಳೆಯರಿಗೆ, ಹೆಚ್ಚು ಆಕ್ರಮಣಕಾರಿ ಶಸ್ತ್ರಚಿಕಿತ್ಸೆಗಳಿಗೆ ಹೋಲಿಸಿದರೆ ಇದು ನಿರ್ಣಾಯಕ ಅಂಶವಾಗಿದೆ.
ಸಾಂಪ್ರದಾಯಿಕ ಕ್ಯುರೆಟ್ಟೇಜ್ನಂತಹ ಕುರುಡು ವಿಧಾನಗಳು ಸಾಮಾನ್ಯವಾಗಿ ಸ್ಥಳೀಯ ಗಾಯಗಳನ್ನು ತಪ್ಪಿಸುತ್ತವೆ. ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ನೈಜ-ಸಮಯದ ದೃಶ್ಯೀಕರಣವನ್ನು ಒದಗಿಸುತ್ತದೆ, ಪಾಲಿಪ್ಸ್, ಫೈಬ್ರಾಯ್ಡ್ಗಳು ಮತ್ತು ಅಂಟಿಕೊಳ್ಳುವಿಕೆಯಂತಹ ಅಸಹಜತೆಗಳನ್ನು ನಿಖರವಾಗಿ ಗುರುತಿಸಲಾಗಿದೆ ಮತ್ತು ಚಿಕಿತ್ಸೆ ನೀಡಲಾಗಿದೆ ಎಂದು ಖಚಿತಪಡಿಸುತ್ತದೆ.
ಸರಳವಾದ ಪಾಲಿಪ್ ತೆಗೆಯುವಿಕೆಯಿಂದ ಹಿಡಿದು ಸಂಕೀರ್ಣವಾದ ಮೈಯೊಮೆಕ್ಟಮಿ ಅಥವಾ ಸೆಪ್ಟಮ್ ರಿಸೆಕ್ಷನ್ ವರೆಗೆ, ಹಿಸ್ಟರೊಸ್ಕೋಪಿಯನ್ನು ವ್ಯಾಪಕ ಶ್ರೇಣಿಯ ಕ್ಲಿನಿಕಲ್ ಸೂಚನೆಗಳಿಗೆ ಅಳವಡಿಸಿಕೊಳ್ಳಬಹುದು. ಈ ನಮ್ಯತೆಯು ಸ್ತ್ರೀರೋಗ ಶಾಸ್ತ್ರದ ಅಭ್ಯಾಸದಲ್ಲಿ ಇದನ್ನು ಅತ್ಯಮೂಲ್ಯ ಸಾಧನಗಳಲ್ಲಿ ಒಂದನ್ನಾಗಿ ಮಾಡುತ್ತದೆ.
ಗರ್ಭಾಶಯದ ಗೋಡೆಯ ಆಕಸ್ಮಿಕ ರಂಧ್ರವು ಅಳವಡಿಕೆ ಅಥವಾ ಶಸ್ತ್ರಚಿಕಿತ್ಸೆಯ ಸಮಯದಲ್ಲಿ ಸಂಭವಿಸಬಹುದು. ಹೆಚ್ಚಿನ ಸಂದರ್ಭಗಳಲ್ಲಿ ದೊಡ್ಡ ಪರಿಣಾಮಗಳಿಲ್ಲದೆ ಗುಣವಾದರೂ, ತೀವ್ರವಾದ ರಂಧ್ರಗಳಿಗೆ ಶಸ್ತ್ರಚಿಕಿತ್ಸೆಯ ದುರಸ್ತಿ ಅಗತ್ಯವಿರಬಹುದು.
ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ನಂತರ ಎಂಡೊಮೆಟ್ರಿಟಿಸ್ ಅಥವಾ ಶ್ರೋಣಿಯ ಸೋಂಕು ಸಾಂದರ್ಭಿಕವಾಗಿ ಸಂಭವಿಸಬಹುದು. ರೋಗನಿರೋಧಕ ಪ್ರತಿಜೀವಕಗಳು ನಿಯಮಿತವಾಗಿ ಅಗತ್ಯವಿಲ್ಲ ಆದರೆ ಹೆಚ್ಚಿನ ಅಪಾಯದ ರೋಗಿಗಳಲ್ಲಿ ಅವುಗಳನ್ನು ಪರಿಗಣಿಸಬಹುದು.
ಶಸ್ತ್ರಚಿಕಿತ್ಸೆಯ ನಂತರ ಸಣ್ಣ ರಕ್ತಸ್ರಾವ ಮತ್ತು ಚುಕ್ಕೆಗಳು ಸಾಮಾನ್ಯ. ದೊಡ್ಡ ಫೈಬ್ರಾಯ್ಡ್ಗಳು ಅಥವಾ ನಾಳೀಯ ಗಾಯಗಳಿಗೆ ಚಿಕಿತ್ಸೆ ನೀಡಿದರೆ, ಅಪರೂಪವಾಗಿದ್ದರೂ, ಅತಿಯಾದ ರಕ್ತಸ್ರಾವ ಸಂಭವಿಸಬಹುದು.
ದ್ರವ ವಿಸ್ತರಣಾ ಮಾಧ್ಯಮವನ್ನು ಬಳಸಿದಾಗ, ರಕ್ತಪ್ರವಾಹಕ್ಕೆ ದ್ರವ ಹೀರಿಕೊಳ್ಳುವ ಅಪಾಯವಿರುತ್ತದೆ. ದ್ರವದ ಒಳಹರಿವು ಮತ್ತು ಹೊರಹರಿವಿನ ಬಗ್ಗೆ ಎಚ್ಚರಿಕೆಯಿಂದ ಮೇಲ್ವಿಚಾರಣೆ ಮಾಡುವುದರಿಂದ ಹೈಪೋನಾಟ್ರೀಮಿಯಾದಂತಹ ತೊಡಕುಗಳ ಸಾಧ್ಯತೆಯನ್ನು ಕಡಿಮೆ ಮಾಡುತ್ತದೆ.
ಸೆಳೆತ, ಲಘು ರಕ್ತಸ್ರಾವ ಮತ್ತು ಸೌಮ್ಯವಾದ ಹೊಟ್ಟೆಯ ಅಸ್ವಸ್ಥತೆ ಸಾಮಾನ್ಯ ಆದರೆ ತಾತ್ಕಾಲಿಕ ಅಡ್ಡಪರಿಣಾಮಗಳು. ಇವು ಸಾಮಾನ್ಯವಾಗಿ ಕೆಲವೇ ದಿನಗಳಲ್ಲಿ ಪರಿಹರಿಸುತ್ತವೆ.
ಅಂತರರಾಷ್ಟ್ರೀಯ ಸುರಕ್ಷತಾ ಮಾರ್ಗಸೂಚಿಗಳನ್ನು ಅನುಸರಿಸುವ ಮೂಲಕ, ಆಧುನಿಕ ಉಪಕರಣಗಳನ್ನು ಬಳಸುವ ಮೂಲಕ ಮತ್ತು ಸರಿಯಾದ ತರಬೇತಿಯನ್ನು ಖಚಿತಪಡಿಸಿಕೊಳ್ಳುವ ಮೂಲಕ, ಹಿಸ್ಟರೊಸ್ಕೋಪಿಯ ಅಪಾಯಗಳನ್ನು ಕಡಿಮೆ ಮಾಡಬಹುದು.
ಹಿಸ್ಟರೋಸ್ಕೋಪಿಯ ವೆಚ್ಚವು ಪ್ರದೇಶ, ಕಾರ್ಯವಿಧಾನದ ಪ್ರಕಾರ ಮತ್ತು ಆರೈಕೆಯ ಸೆಟ್ಟಿಂಗ್ಗಳ ಆಧಾರದ ಮೇಲೆ ಬದಲಾಗುತ್ತದೆ. ರೋಗಿಗಳು ಮತ್ತು ಆಸ್ಪತ್ರೆ ಖರೀದಿದಾರರಿಗೆ, ಸೇವೆಯು ರೋಗನಿರ್ಣಯದ ಹಿಸ್ಟರೋಸ್ಕೋಪಿ ಅಥವಾ ಶಸ್ತ್ರಚಿಕಿತ್ಸಾ ಹಿಸ್ಟರೋಸ್ಕೋಪಿ (ಉದಾ, ಹಿಸ್ಟರೋಸ್ಕೋಪಿ ಡಿ & ಸಿ ಅಥವಾ ಹಿಸ್ಟರೋಸ್ಕೋಪಿ ಪಾಲಿಪೆಕ್ಟಮಿ), ಹಾಗೆಯೇ ಅರಿವಳಿಕೆ, ಸೌಲಭ್ಯ ಶುಲ್ಕಗಳು ಮತ್ತು ಚೇತರಿಕೆಯ ಅಗತ್ಯತೆಗಳ ಮೇಲೆ ಬೆಲೆ ಪ್ರಭಾವ ಬೀರುತ್ತದೆ.
ಯುನೈಟೆಡ್ ಸ್ಟೇಟ್ಸ್: ರೋಗನಿರ್ಣಯದ ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಸಾಮಾನ್ಯವಾಗಿ $1,000–$3,000 ವರೆಗೆ ಇರುತ್ತದೆ; ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಡಿ&ಸಿ ಅಥವಾ ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಪಾಲಿಪೆಕ್ಟಮಿಯಂತಹ ಶಸ್ತ್ರಚಿಕಿತ್ಸಾ ವಿಧಾನಗಳು ಸಾಮಾನ್ಯವಾಗಿ $3,000–$5,000 ವರೆಗೆ ಇರುತ್ತದೆ.
ಯುರೋಪ್: ಸಾರ್ವಜನಿಕ ವ್ಯವಸ್ಥೆಗಳು ಆಗಾಗ್ಗೆ ವೈದ್ಯಕೀಯವಾಗಿ ಅಗತ್ಯವಾದ ಕಾರ್ಯವಿಧಾನಗಳನ್ನು ಒಳಗೊಂಡಿರುತ್ತವೆ; ಖಾಸಗಿ ಶುಲ್ಕಗಳು ಸಾಮಾನ್ಯವಾಗಿ €800–€2,500 ರಷ್ಟಿರುತ್ತವೆ.
ಏಷ್ಯಾ-ಪೆಸಿಫಿಕ್: ನಗರ ಮತ್ತು ಸೌಲಭ್ಯದ ಮಟ್ಟವನ್ನು ಅವಲಂಬಿಸಿ ರೋಗನಿರ್ಣಯದ ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಸಾಮಾನ್ಯವಾಗಿ $500–$1,500 ರಷ್ಟಿದೆ.
ಅಭಿವೃದ್ಧಿ ಹೊಂದುತ್ತಿರುವ ಪ್ರದೇಶಗಳು: ಪ್ರವೇಶ ಸೀಮಿತವಾಗಿರಬಹುದು; ಔಟ್ರೀಚ್ ಕಾರ್ಯಕ್ರಮಗಳು ಮತ್ತು ಮೊಬೈಲ್ ಚಿಕಿತ್ಸಾಲಯಗಳು ಲಭ್ಯತೆಯನ್ನು ವಿಸ್ತರಿಸುತ್ತಿವೆ.
ಅಸಹಜ ಗರ್ಭಾಶಯದ ರಕ್ತಸ್ರಾವ (AUB), ಬಂಜೆತನದ ಮೌಲ್ಯಮಾಪನಗಳು ಅಥವಾ ಶಂಕಿತ ಗರ್ಭಾಶಯದ ರೋಗಶಾಸ್ತ್ರಕ್ಕೆ ನಡೆಸಿದಾಗ, ಹಿಸ್ಟರೊಸ್ಕೋಪಿಯನ್ನು ಹೆಚ್ಚಾಗಿ ವೈದ್ಯಕೀಯವಾಗಿ ಅಗತ್ಯವೆಂದು ಪರಿಗಣಿಸಲಾಗುತ್ತದೆ ಮತ್ತು ಇದನ್ನು ಒಳಗೊಳ್ಳಬಹುದು.
ಚುನಾಯಿತ ಅಥವಾ ಸೌಂದರ್ಯವರ್ಧಕ ಸೂಚನೆಗಳು ರೋಗಿಗಳಿಗೆ ಹೆಚ್ಚಿನ ಜೇಬಿನಿಂದ ವೆಚ್ಚವನ್ನು ಒಳಗೊಂಡಿರಬಹುದು.
ಕಚೇರಿ ಆಧಾರಿತ ಹಿಸ್ಟರೊಸ್ಕೋಪಿ: ಮಿನಿ-ಹಿಸ್ಟರೊಸ್ಕೋಪ್ಗಳನ್ನು ಬಳಸುತ್ತದೆ; ಸಾಮಾನ್ಯವಾಗಿ ಕಡಿಮೆ ವೆಚ್ಚ, ವೇಗವಾದ ವಹಿವಾಟು ಮತ್ತು ರೋಗನಿರ್ಣಯದ ಪ್ರಕರಣಗಳು ಅಥವಾ ಸಣ್ಣ ಶಸ್ತ್ರಚಿಕಿತ್ಸಾ ಕೆಲಸಗಳಿಗೆ ಕನಿಷ್ಠ ಅಥವಾ ಅರಿವಳಿಕೆ ಇಲ್ಲ.
ಆಸ್ಪತ್ರೆ ಆಧಾರಿತ ಹಿಸ್ಟರೊಸ್ಕೋಪಿ: ಸಾಮಾನ್ಯ ಅರಿವಳಿಕೆ, OR ಸಮಯ ಮತ್ತು ಮೇಲ್ವಿಚಾರಣೆಯ ಚೇತರಿಕೆಯ ಅಗತ್ಯವಿರುವ ಸಂಕೀರ್ಣ ಶಸ್ತ್ರಚಿಕಿತ್ಸಾ ಹಿಸ್ಟರೊಸ್ಕೋಪಿಗೆ (ಉದಾ, ದೊಡ್ಡ ಫೈಬ್ರಾಯ್ಡ್ಗಳು, ವ್ಯಾಪಕ ಅಂಟಿಕೊಳ್ಳುವಿಕೆಗಳು) ಆದ್ಯತೆ ನೀಡಲಾಗುತ್ತದೆ.
ಒಳರೋಗಿಗಳಿಂದ ಕಚೇರಿ ಆಧಾರಿತ ಸೆಟ್ಟಿಂಗ್ಗಳಿಗೆ ಸೂಕ್ತವಾದ ಪ್ರಕರಣಗಳನ್ನು ಬದಲಾಯಿಸುವುದರಿಂದ ಆರೈಕೆಯ ಒಟ್ಟು ವೆಚ್ಚ ಕಡಿಮೆಯಾಗುತ್ತದೆ ಮತ್ತು ರೋಗಿಗಳ ಥ್ರೋಪುಟ್ ಹೆಚ್ಚಾಗುತ್ತದೆ.
ಮರುಬಳಕೆ ಮಾಡಬಹುದಾದ ಹಿಸ್ಟರೊಸ್ಕೋಪ್ಗಳು, ದ್ರವ ನಿರ್ವಹಣೆ ಮತ್ತು ಇಮೇಜಿಂಗ್ನಲ್ಲಿ ಹೂಡಿಕೆ ಮಾಡುವುದರಿಂದ ತೊಡಕುಗಳ ಪ್ರಮಾಣ ಮತ್ತು ಮರು ಪ್ರವೇಶವನ್ನು ಕಡಿಮೆ ಮಾಡಬಹುದು.
ಸಲಕರಣೆಗಳ ವೆಚ್ಚಗಳು: ಉತ್ತಮ ಗುಣಮಟ್ಟದ ಹಿಸ್ಟರೊಸ್ಕೋಪ್ಗಳು, ರೆಸೆಕ್ಟೋಸ್ಕೋಪ್ಗಳು ಮತ್ತು ದೃಶ್ಯೀಕರಣ ವ್ಯವಸ್ಥೆಗಳಿಗೆ ಆರಂಭಿಕ ಬಂಡವಾಳದ ಅಗತ್ಯವಿರುತ್ತದೆ; ಬಿಸಾಡಬಹುದಾದ ವಸ್ತುಗಳು ಮತ್ತು ನಿರ್ವಹಣೆಯು ಪುನರಾವರ್ತಿತ ವೆಚ್ಚಗಳನ್ನು ಸೇರಿಸುತ್ತದೆ.
ತರಬೇತಿ: ಸುರಕ್ಷಿತ, ಪರಿಣಾಮಕಾರಿ ಶಸ್ತ್ರಚಿಕಿತ್ಸಾ ಹಿಸ್ಟರೊಸ್ಕೋಪಿಗೆ ವಿಶೇಷ ಕೌಶಲ್ಯಗಳು ಬೇಕಾಗುತ್ತವೆ; ಕಡಿಮೆ ಸಂಪನ್ಮೂಲ ಹೊಂದಿರುವ ಸೆಟ್ಟಿಂಗ್ಗಳಲ್ಲಿ ಸೀಮಿತ ತರಬೇತಿ ಪ್ರವೇಶವು ದತ್ತು ಸ್ವೀಕಾರವನ್ನು ನಿರ್ಬಂಧಿಸುತ್ತದೆ.
ಮೂಲಸೌಕರ್ಯ: OR ಲಭ್ಯತೆ, ಅರಿವಳಿಕೆ ಬೆಂಬಲ ಮತ್ತು ಪೂರೈಕೆ ಸರಪಳಿಯ ವಿಶ್ವಾಸಾರ್ಹತೆಯು ಸೇವಾ ಸಾಮರ್ಥ್ಯದ ಮೇಲೆ ಪರಿಣಾಮ ಬೀರುತ್ತದೆ.
ರೋಗಿಯ ಅರಿವು: ಅನೇಕ ರೋಗಿಗಳಿಗೆ ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಎಂದರೇನು ಅಥವಾ ಅದರ ಪ್ರಯೋಜನಗಳ ಬಗ್ಗೆ ತಿಳಿದಿಲ್ಲ; ಶಿಕ್ಷಣವು ಹೀರಿಕೊಳ್ಳುವಿಕೆಯನ್ನು ಸುಧಾರಿಸುತ್ತದೆ.
ಉತ್ತರ ಅಮೆರಿಕಾ: ಹೆಚ್ಚಿನ ಅಳವಡಿಕೆ; ವ್ಯಾಪಕವಾದ ಕಚೇರಿ ಆಧಾರಿತ ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಮತ್ತು ಮುಂದುವರಿದ ಚಿತ್ರಣ.
ಯುರೋಪ್: ಸಾರ್ವಜನಿಕ ವ್ಯವಸ್ಥೆಗಳಲ್ಲಿ ವಿಶಾಲ ಏಕೀಕರಣ; ಯುಕೆ, ಜರ್ಮನಿ, ಇಟಲಿ ಮತ್ತು ಇತರ ದೇಶಗಳಲ್ಲಿ ಕಚೇರಿ ಹಿಸ್ಟರೊಸ್ಕೋಪಿಯ ಬಲವಾದ ಬಳಕೆ.
ಏಷ್ಯಾ-ಪೆಸಿಫಿಕ್: ಚೀನಾ, ಭಾರತ, ದಕ್ಷಿಣ ಕೊರಿಯಾ ಮತ್ತು ಆಗ್ನೇಯ ಏಷ್ಯಾದಲ್ಲಿನ ಫಲವತ್ತತೆ ಕೇಂದ್ರಗಳು ಮತ್ತು ಖಾಸಗಿ ಆಸ್ಪತ್ರೆಗಳಿಂದ ತ್ವರಿತ ಬೆಳವಣಿಗೆ.
ಆಫ್ರಿಕಾ ಮತ್ತು ಲ್ಯಾಟಿನ್ ಅಮೆರಿಕ: ಅಸಮಾನ ಪ್ರವೇಶ; ಸರ್ಕಾರಿ ಉಪಕ್ರಮಗಳು ಮತ್ತು NGO ಪಾಲುದಾರಿಕೆಗಳು ಸೇವೆಗಳನ್ನು ವಿಸ್ತರಿಸುತ್ತಿವೆ.
ಇತ್ತೀಚಿನ ಆವಿಷ್ಕಾರಗಳು ರೋಗನಿರ್ಣಯದ ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಮತ್ತು ಶಸ್ತ್ರಚಿಕಿತ್ಸಾ ಹಿಸ್ಟರೊಸ್ಕೋಪಿಯನ್ನು ಸುರಕ್ಷಿತ, ವೇಗವಾದ ಮತ್ತು ಹೆಚ್ಚು ಆರಾಮದಾಯಕವಾಗಿಸುವ ಗುರಿಯನ್ನು ಹೊಂದಿವೆ, ಜೊತೆಗೆ ದೃಶ್ಯೀಕರಣ ಮತ್ತು ದಕ್ಷತೆಯನ್ನು ಸುಧಾರಿಸುತ್ತವೆ.
ಮಿನಿ-ಹಿಸ್ಟರೊಸ್ಕೋಪ್ಗಳು ರೋಗನಿರ್ಣಯದ ಹಿಸ್ಟರೊಸ್ಕೋಪಿಯನ್ನು ಸಕ್ರಿಯಗೊಳಿಸುತ್ತವೆ ಮತ್ತು ಸಾಮಾನ್ಯ ಅರಿವಳಿಕೆ ಇಲ್ಲದೆ ಮಧ್ಯಸ್ಥಿಕೆಗಳನ್ನು ಆಯ್ಕೆ ಮಾಡುತ್ತವೆ, ವೆಚ್ಚ ಮತ್ತು ಚೇತರಿಕೆಯ ಸಮಯವನ್ನು ಕಡಿಮೆ ಮಾಡುತ್ತದೆ.
HD ಮತ್ತು ಡಿಜಿಟಲ್ ಹಿಸ್ಟರೊಸ್ಕೋಪ್ಗಳು ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಪಾಲಿಪೆಕ್ಟಮಿ ಮತ್ತು ಅಡೆಸಿಯೋಲಿಸಿಸ್ಗೆ ಪತ್ತೆ ಮತ್ತು ಮಾರ್ಗದರ್ಶನವನ್ನು ಹೆಚ್ಚಿಸುವ ಸ್ಪಷ್ಟ ಚಿತ್ರಗಳನ್ನು ಒದಗಿಸುತ್ತವೆ.
ಹಿಸ್ಟರೊಸ್ಕೋಪಿಕ್ ಕಾರ್ಯವಿಧಾನದ ಸಮಯದಲ್ಲಿ ದ್ರವದ ಓವರ್ಲೋಡ್ ಅಪಾಯವನ್ನು ಕಡಿಮೆ ಮಾಡುವ ಮೂಲಕ ಸ್ವಯಂಚಾಲಿತ ಒಳಹರಿವು/ಹೊರಹರಿವಿನ ಮೇಲ್ವಿಚಾರಣೆ ಸುರಕ್ಷತೆಯನ್ನು ಸುಧಾರಿಸುತ್ತದೆ.
ಉದಯೋನ್ಮುಖ ವೇದಿಕೆಗಳು ಸಂಕೀರ್ಣ ಗರ್ಭಾಶಯದ ಛೇದನಗಳಿಗೆ ಸುಧಾರಿತ ಆಳ ಗ್ರಹಿಕೆ ಮತ್ತು ಉಪಕರಣ ನಿಯಂತ್ರಣವನ್ನು ನೀಡುತ್ತವೆ.
ಎಂಡೊಮೆಟ್ರಿಯಲ್ ಪಾಲಿಪ್ಸ್, ಸಬ್ಮ್ಯೂಕೋಸಲ್ ಫೈಬ್ರಾಯ್ಡ್ಗಳು ಮತ್ತು ಅಂಟಿಕೊಳ್ಳುವಿಕೆಗಳ ನೈಜ-ಸಮಯದ ಗುರುತಿಸುವಿಕೆಯನ್ನು ಬೆಂಬಲಿಸಲು AI-ನೆರವಿನ ಚಿತ್ರ ವಿಶ್ಲೇಷಣೆಯನ್ನು ಅನ್ವೇಷಿಸಲಾಗುತ್ತಿದೆ.
ಹಿಸ್ಟರೊಸ್ಕೋಪಿಕ್ ಕಾರ್ಯವಿಧಾನಗಳ ಪರಿಣಾಮಕಾರಿತ್ವ ಮತ್ತು ಸುರಕ್ಷತೆಯು ಅಂತರರಾಷ್ಟ್ರೀಯ ಮಾರ್ಗಸೂಚಿಗಳ ಕಟ್ಟುನಿಟ್ಟಿನ ಅನುಸರಣೆ ಮತ್ತು ಅವುಗಳನ್ನು ನಿರ್ವಹಿಸುವ ತಜ್ಞರ ಅರ್ಹತೆಗಳನ್ನು ಅವಲಂಬಿಸಿರುತ್ತದೆ.
ವೃತ್ತಿಪರ ತರಬೇತಿ
ಎಂಡೋಸ್ಕೋಪಿಕ್ ತಂತ್ರಗಳಲ್ಲಿ ಔಪಚಾರಿಕ ತರಬೇತಿ ಪಡೆದ ಸ್ತ್ರೀರೋಗತಜ್ಞರು ಹಿಸ್ಟರೊಸ್ಕೋಪಿಯನ್ನು ನಡೆಸಬೇಕು. ನಿರಂತರ ಶಿಕ್ಷಣ ಮತ್ತು ಸಿಮ್ಯುಲೇಶನ್ ಆಧಾರಿತ ಅಭ್ಯಾಸವು ತೊಡಕುಗಳ ಅಪಾಯವನ್ನು ಕಡಿಮೆ ಮಾಡುತ್ತದೆ ಮತ್ತು ಫಲಿತಾಂಶಗಳನ್ನು ಸುಧಾರಿಸುತ್ತದೆ.
ಪುರಾವೆ ಆಧಾರಿತ ಪ್ರೋಟೋಕಾಲ್ಗಳು
ಅಮೇರಿಕನ್ ಕಾಲೇಜ್ ಆಫ್ ಅಬ್ಸ್ಟೆಟ್ರಿಶಿಯನ್ಸ್ ಅಂಡ್ ಗೈನಕಾಲಜಿಸ್ಟ್ಸ್ (ACOG) ಮತ್ತು ಯುರೋಪಿಯನ್ ಸೊಸೈಟಿ ಫಾರ್ ಗೈನಕಾಲಜಿಕಲ್ ಎಂಡೋಸ್ಕೋಪಿ (ESGE) ನಂತಹ ಸಂಸ್ಥೆಗಳು ರೋಗನಿರ್ಣಯ ಮತ್ತು ಆಪರೇಟಿವ್ ಹಿಸ್ಟರೊಸ್ಕೋಪಿಗೆ ವಿವರವಾದ ಶಿಫಾರಸುಗಳನ್ನು ಪ್ರಕಟಿಸುತ್ತವೆ. ಈ ಪ್ರೋಟೋಕಾಲ್ಗಳು ರೋಗಿಯ ಆಯ್ಕೆ, ದ್ರವ ನಿರ್ವಹಣೆ ಮತ್ತು ಶಸ್ತ್ರಚಿಕಿತ್ಸಾ ಸುರಕ್ಷತೆಯ ಕುರಿತು ನಿರ್ಧಾರಗಳನ್ನು ಮಾರ್ಗದರ್ಶಿಸುತ್ತವೆ.
ಗುಣಮಟ್ಟದ ಭರವಸೆ
ಕಟ್ಟುನಿಟ್ಟಾದ ಕ್ರಿಮಿನಾಶಕ, ಉಪಕರಣಗಳ ನಿರ್ವಹಣೆ ಮತ್ತು ಮೇಲ್ವಿಚಾರಣಾ ಮಾನದಂಡಗಳನ್ನು ಜಾರಿಗೊಳಿಸುವ ಆಸ್ಪತ್ರೆಗಳು ಹೆಚ್ಚಿನ ಸುರಕ್ಷತಾ ಮಟ್ಟವನ್ನು ಸಾಧಿಸುತ್ತವೆ. ಸುಧಾರಿತ ದ್ರವ ನಿರ್ವಹಣಾ ವ್ಯವಸ್ಥೆಗಳು ಮತ್ತು ಪ್ರಮಾಣೀಕೃತ ವರದಿ ಮಾಡುವಿಕೆಯು ಕಾರ್ಯವಿಧಾನದ ಸ್ಥಿರತೆಯನ್ನು ಸುಧಾರಿಸುತ್ತದೆ.
ರೋಗಿ-ಕೇಂದ್ರಿತ ಆರೈಕೆ
ಮಾಹಿತಿಯುಕ್ತ ಒಪ್ಪಿಗೆ, ಅಪಾಯಗಳು ಮತ್ತು ಪರ್ಯಾಯಗಳ ಬಗ್ಗೆ ಪಾರದರ್ಶಕ ಸಂವಹನ ಮತ್ತು ವೈಯಕ್ತಿಕ ಚಿಕಿತ್ಸಾ ಯೋಜನೆ ರೋಗಿಗಳು ಮತ್ತು ಆರೋಗ್ಯ ಪೂರೈಕೆದಾರರ ನಡುವೆ ನಂಬಿಕೆಯನ್ನು ಬಲಪಡಿಸುತ್ತದೆ.
ಮಾನ್ಯತೆ ಪಡೆದ ಮಾರ್ಗಸೂಚಿಗಳನ್ನು ಅನುಸರಿಸುವ ಮೂಲಕ ಮತ್ತು ವೃತ್ತಿಪರ ಮಾನದಂಡಗಳನ್ನು ಕಾಯ್ದುಕೊಳ್ಳುವ ಮೂಲಕ, ಪ್ರಪಂಚದಾದ್ಯಂತ ಗರ್ಭಾಶಯದ ಕಾಯಿಲೆಗಳನ್ನು ಪತ್ತೆಹಚ್ಚಲು ಮತ್ತು ಚಿಕಿತ್ಸೆ ನೀಡಲು ಹಿಸ್ಟರೊಸ್ಕೋಪಿಯನ್ನು ಚಿನ್ನದ ಮಾನದಂಡವೆಂದು ಪರಿಗಣಿಸಲಾಗುತ್ತಿದೆ.
ಗರ್ಭಾಶಯದ ಗರ್ಭಾಶಯದ ಸ್ಥಿತಿಗಳನ್ನು ಮೌಲ್ಯಮಾಪನ ಮಾಡಲು ಮತ್ತು ಚಿಕಿತ್ಸೆ ನೀಡಲು ಕನಿಷ್ಠ ಆಕ್ರಮಣಕಾರಿ, ಹೆಚ್ಚು ನಿಖರವಾದ ವಿಧಾನವನ್ನು ನೀಡುವ ಮೂಲಕ ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಸ್ತ್ರೀರೋಗ ಶಾಸ್ತ್ರದ ಅಭ್ಯಾಸದಲ್ಲಿ ಕ್ರಾಂತಿಯನ್ನುಂಟು ಮಾಡಿದೆ. ರೋಗನಿರ್ಣಯದ ಹಿಸ್ಟರೊಸ್ಕೋಪಿಯಿಂದ ಹಿಡಿದು ಡಿ & ಸಿ, ಪಾಲಿಪೆಕ್ಟಮಿ ಮತ್ತು ಮೈಯೊಮೆಕ್ಟಮಿಯಂತಹ ಮುಂದುವರಿದ ಶಸ್ತ್ರಚಿಕಿತ್ಸಾ ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಕಾರ್ಯವಿಧಾನಗಳವರೆಗೆ, ಈ ತಂತ್ರವು ರೋಗಿಯ ಫಲಿತಾಂಶಗಳನ್ನು ಸುಧಾರಿಸುತ್ತದೆ ಮತ್ತು ಚೇತರಿಕೆಯ ಸಮಯವನ್ನು ಕಡಿಮೆ ಮಾಡುತ್ತದೆ ಮತ್ತು ಫಲವತ್ತತೆಯನ್ನು ಸಂರಕ್ಷಿಸುತ್ತದೆ.
ಆಸ್ಪತ್ರೆಗಳು ಮತ್ತು ಚಿಕಿತ್ಸಾಲಯಗಳಿಗೆ, ಹಿಸ್ಟರೊಸ್ಕೋಪಿಕ್ ಉಪಕರಣಗಳು ಮತ್ತು ಸಿಬ್ಬಂದಿ ತರಬೇತಿಯಲ್ಲಿ ಹೂಡಿಕೆ ಮಾಡುವುದು ವೈದ್ಯಕೀಯ ಅವಶ್ಯಕತೆಯಷ್ಟೇ ಅಲ್ಲ, ರೋಗಿಗಳ ಆರೈಕೆಯನ್ನು ಹೆಚ್ಚಿಸುವ, ಸಂಪನ್ಮೂಲಗಳನ್ನು ಉತ್ತಮಗೊಳಿಸುವ ಮತ್ತು ಸಾಂಸ್ಥಿಕ ಖ್ಯಾತಿಯನ್ನು ಬಲಪಡಿಸುವ ಕಾರ್ಯತಂತ್ರದ ನಿರ್ಧಾರವೂ ಆಗಿದೆ. ರೋಗಿಗಳಿಗೆ, ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಭರವಸೆ ನೀಡುತ್ತದೆ - ಗರ್ಭಾಶಯದ ಆರೋಗ್ಯಕ್ಕೆ ಸುರಕ್ಷಿತ, ನಿಖರ ಮತ್ತು ಆಧುನಿಕ ವಿಧಾನವನ್ನು ನೀಡುತ್ತದೆ.
ತಂತ್ರಜ್ಞಾನವು ಮಿನಿ-ಹಿಸ್ಟರೊಸ್ಕೋಪ್ಗಳು, ಡಿಜಿಟಲ್ ಇಮೇಜಿಂಗ್ ಮತ್ತು AI-ಚಾಲಿತ ರೋಗನಿರ್ಣಯಗಳೊಂದಿಗೆ ಮುಂದುವರೆದಂತೆ, ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ವಿಶ್ವಾದ್ಯಂತ ಮಹಿಳಾ ಆರೋಗ್ಯ ರಕ್ಷಣೆಯ ಮೂಲಾಧಾರವಾಗಿ ವಿಕಸನಗೊಳ್ಳುವುದನ್ನು ಮುಂದುವರಿಸುತ್ತದೆ, ನಿಖರವಾದ ರೋಗನಿರ್ಣಯ ಮತ್ತು ಪರಿಣಾಮಕಾರಿ ಚಿಕಿತ್ಸೆಯ ನಡುವಿನ ಅಂತರವನ್ನು ಕಡಿಮೆ ಮಾಡುತ್ತದೆ.
ಗರ್ಭಾಶಯದೊಳಗಿನ ಅಸಹಜ ರಕ್ತಸ್ರಾವ, ಗರ್ಭಾಶಯದ ಪಾಲಿಪ್ಸ್, ಫೈಬ್ರಾಯ್ಡ್ಗಳು, ಅಂಟಿಕೊಳ್ಳುವಿಕೆಗಳು ಮತ್ತು ಜನ್ಮಜಾತ ವೈಪರೀತ್ಯಗಳಂತಹ ಪರಿಸ್ಥಿತಿಗಳನ್ನು ಪತ್ತೆಹಚ್ಚಲು ಮತ್ತು ಚಿಕಿತ್ಸೆ ನೀಡಲು ಹಿಸ್ಟರೊಸ್ಕೋಪಿಯನ್ನು ಬಳಸಲಾಗುತ್ತದೆ. ಬಂಜೆತನದ ಮೌಲ್ಯಮಾಪನ ಮತ್ತು ಮರುಕಳಿಸುವ ಗರ್ಭಧಾರಣೆಯ ನಷ್ಟ ನಿರ್ವಹಣೆಯಲ್ಲಿ ಇದು ಒಂದು ಪ್ರಮುಖ ಸಾಧನವಾಗಿದೆ.
ಗರ್ಭಾಶಯದ ಕುಹರವನ್ನು ಪರೀಕ್ಷಿಸಲು ಮತ್ತು ಅಸಹಜತೆಗಳನ್ನು ಪತ್ತೆಹಚ್ಚಲು ರೋಗನಿರ್ಣಯದ ಹಿಸ್ಟರೊಸ್ಕೋಪಿಯನ್ನು ನಡೆಸಲಾಗುತ್ತದೆ, ಆದರೆ ಶಸ್ತ್ರಚಿಕಿತ್ಸಾ ಹಿಸ್ಟರೊಸ್ಕೋಪಿ (ಆಪರೇಟಿವ್ ಹಿಸ್ಟರೊಸ್ಕೋಪಿ) ವೈದ್ಯರಿಗೆ ಫೈಬ್ರಾಯ್ಡ್ಗಳನ್ನು ತೆಗೆದುಹಾಕುವುದು ಅಥವಾ ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಪಾಲಿಪೆಕ್ಟಮಿ ಮಾಡುವಂತಹ ಈ ಅಸಹಜತೆಗಳಿಗೆ ಚಿಕಿತ್ಸೆ ನೀಡಲು ಅನುವು ಮಾಡಿಕೊಡುತ್ತದೆ.
ಹಿಸ್ಟರೊಸ್ಕೋಪ್ ಎನ್ನುವುದು ತೆಳುವಾದ, ಬೆಳಕು ತುಂಬಿದ ಎಂಡೋಸ್ಕೋಪಿಕ್ ಉಪಕರಣವಾಗಿದ್ದು, ಗರ್ಭಕಂಠದ ಮೂಲಕ ಗರ್ಭಾಶಯದೊಳಗೆ ಸೇರಿಸಲಾಗುತ್ತದೆ. ಇದು ಕ್ಯಾಮೆರಾ ಮತ್ತು ಬೆಳಕಿನ ಮೂಲವನ್ನು ಹೊಂದಿದ್ದು, ಗರ್ಭಾಶಯದ ಕುಹರದ ನೇರ ದೃಶ್ಯೀಕರಣವನ್ನು ಅನುಮತಿಸುತ್ತದೆ ಮತ್ತು ಅಗತ್ಯವಿದ್ದಾಗ ಶಸ್ತ್ರಚಿಕಿತ್ಸಾ ಉಪಕರಣಗಳಿಗೆ ಮಾರ್ಗದರ್ಶನ ನೀಡುತ್ತದೆ.
ಹಿಸ್ಟರೊಸ್ಕೋಪಿ D&C ಹಿಸ್ಟರೊಸ್ಕೋಪಿಕ್ ದೃಶ್ಯೀಕರಣವನ್ನು ಹಿಗ್ಗುವಿಕೆ ಮತ್ತು ಕ್ಯುರೆಟ್ಟೇಜ್ನೊಂದಿಗೆ ಸಂಯೋಜಿಸುತ್ತದೆ. ಹಿಸ್ಟರೊಸ್ಕೋಪ್ ಎಂಡೊಮೆಟ್ರಿಯಲ್ ಅಂಗಾಂಶವನ್ನು ತೆಗೆದುಹಾಕಲು ಮಾರ್ಗದರ್ಶನ ನೀಡಲು ಸಹಾಯ ಮಾಡುತ್ತದೆ, ಇದು ಬ್ಲೈಂಡ್ ಕ್ಯುರೆಟ್ಟೇಜ್ಗಿಂತ ಕಾರ್ಯವಿಧಾನವನ್ನು ಹೆಚ್ಚು ನಿಖರ ಮತ್ತು ಸುರಕ್ಷಿತವಾಗಿಸುತ್ತದೆ.
ರೋಗನಿರ್ಣಯದ ಹಿಸ್ಟರೊಸ್ಕೋಪಿ ಸಮಯದಲ್ಲಿ ಹೆಚ್ಚಿನ ಮಹಿಳೆಯರು ಸೌಮ್ಯ ಅಸ್ವಸ್ಥತೆಯನ್ನು ಮಾತ್ರ ಅನುಭವಿಸುತ್ತಾರೆ. ಆರಾಮ ಮತ್ತು ಸುರಕ್ಷತೆಯನ್ನು ಖಚಿತಪಡಿಸಿಕೊಳ್ಳಲು ಶಸ್ತ್ರಚಿಕಿತ್ಸಾ ವಿಧಾನಗಳಿಗೆ ಸ್ಥಳೀಯ, ಪ್ರಾದೇಶಿಕ ಅಥವಾ ಸಾಮಾನ್ಯ ಅರಿವಳಿಕೆ ಅಗತ್ಯವಿರಬಹುದು.
ಕೃತಿಸ್ವಾಮ್ಯ © 2025. ಗೀಕ್ವಾಲ್ಯೂ ಎಲ್ಲ ಹಕ್ಕುಗಳನ್ನು ಕಾಯ್ದಿರಿಸಲಾಗಿದೆ.ತಾಂತ್ರಿಕ ಸಹಾಯ: TiaoQingCMS