Medical Hysteroscopy Equipment
This system provides HD imaging for uterine endoscopy medical endoscopes, enabling clear visualization during hysteroscopic diagnostics. Optimizes gynecological endoscope medical procedures through physical controls and compact design.
Technical Specifications
HD imaging resolution (1920×1080)
Physical control knobs for precise operation
Integrated carrying handle
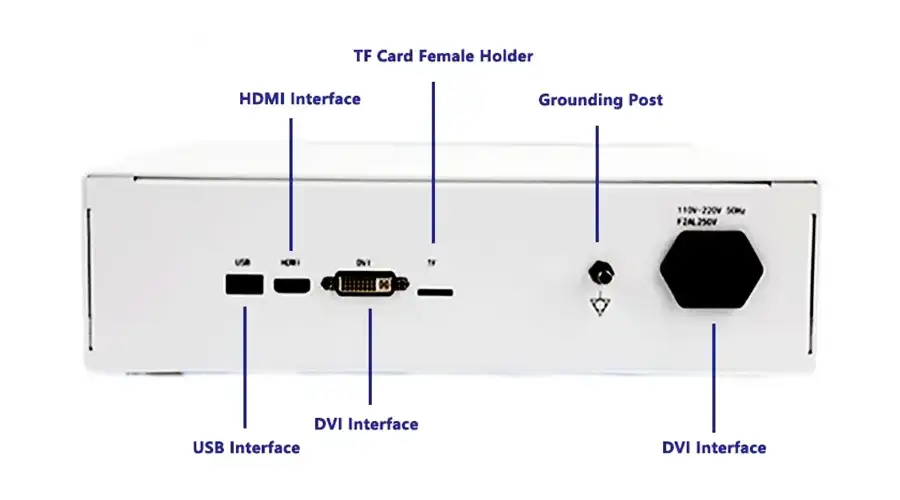
HDMI/USB video outputs
Compact desktop form factor
Clinical Applications
Uterine cavity examination: Detailed mucosal visualization
Polyp detection: Identification of intrauterine abnormalities
Diagnostic procedures: Efficient gynecological workflows
Operational Features
Corrosion-resistant housing for sterilization compliance
Ergonomic interface for clinical use
Stable performance for hysteroscopic endoscopy medical endoscopes
Focused exclusively on core uterine endoscopic imaging with optimized control and mobility.

Strong Compatibility
Compatible with Gastrointestinal Endoscopes, Urological Endoscopes, Bronchoscopes, Hysteroscopes,Arthroscopes, Cystoscopes, Laryngoscopes, Choledochoscopes, Strong Compatibility.
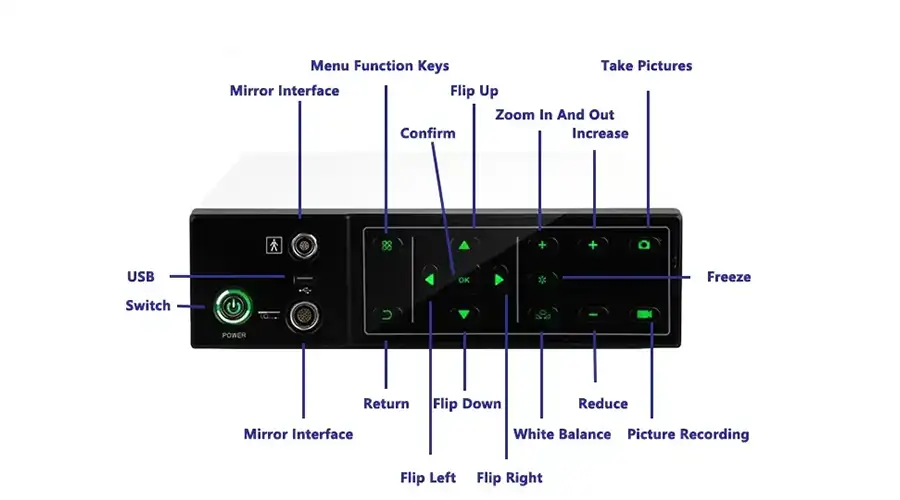
Capture
Freeze
Zoom In/Out
Image Settings
REC
Brightness: 5 levels
WB
Multi-Interface
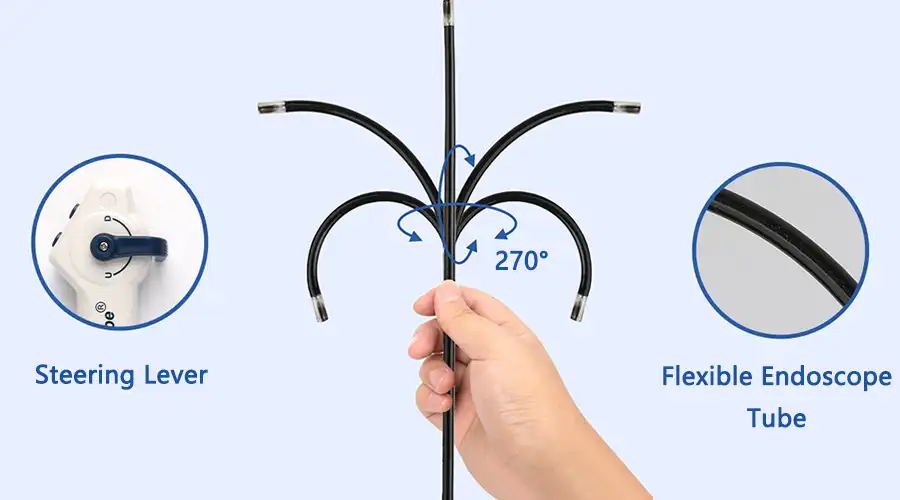
1920*1200 Pixel Resolution Image Clarity
with Detailed Vascular Visualization for Real-Time Diagnosis

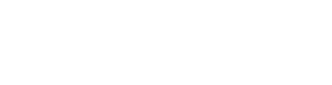
360-Degree Blind Spot-Free Rotation
Flexible 360-degree lateral rotation
Eliminates visual blind spots effectively
Dual LED Lighting
5 adjustable brightness levels, Brightest at Level 5
gradually dimming to OFF
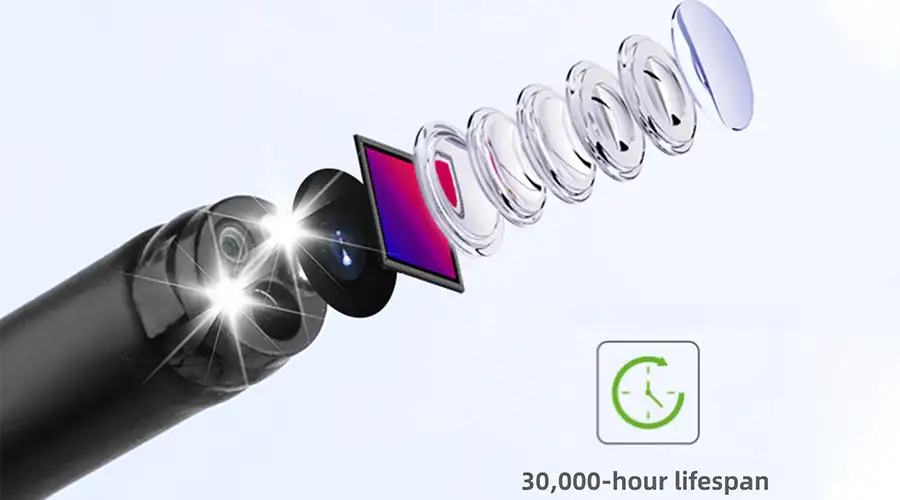
Brightest at Level 5
Brightness: 5 levels
OFF
Level 1
Level 2
Level 6
Level 4
Level 5
Manual 5x Image Magnification
Enhances detail detection
for exceptional results


Photo/Video Operation One-touch control
Capture via host unit buttons or
handpiece shutter control
IP67-Rated High-definition waterproof lens
Sealed with special materials
for water, oil, and corrosion resistance

Hysteroscopy, as the gold standard for minimally invasive gynecological diagnosis and treatment, enables visual diagnosis and precise treatment of the intrauterine environment through natural cavities. The following is a comprehensive analysis of modern hysteroscopy technology from seven dimensions:
I. Core technology and equipment composition
Imaging system
4K ultra-high-definition endoscope (resolution ≥3840×2160)
Optical zoom (3-50 times continuous magnification)
NBI narrow-band imaging technology (enhanced vascular display)
Energy system
Bipolar electrosurgical resection (safety threshold <200W)
Holmium laser (wavelength 2100nm)
Radiofrequency ablation (controllable temperature 42-70℃)
II. Clinical application matrix
Disease field Diagnostic value Treatment breakthrough
Abnormal uterine bleeding Positioning bleeding focus (sensitivity 98%) Endometrial resection/ablation
Infertility Assessment of fallopian tube opening status Intrauterine adhesion decomposition (success rate 85%)
Uterine malformation Three-dimensional reconstruction of uterine cavity morphology Septum resection (postoperative pregnancy rate ↑40%)
Intrauterine foreign body Accurate positioning of residual tissue Embryo removal (retaining reproductive function)
III. Comparison of innovative equipment
Charts
Codes
IV. Optimization of surgical procedures
Preoperative preparation
3-7 days after menstruation
Cervical pretreatment (misoprostol 400μg)
Uterine distention pressure control (80-100mmHg)
V. Complication prevention and control system
Fluid overload
Real-time monitoring: liquid difference <1000ml
Uterine distention medium: saline (conductive) vs. Glucose (non-conductive)
Uterine perforation
Navigation warning system (accuracy 0.5mm)
Intraoperative ultrasound monitoring
VI. Cutting-edge technology breakthroughs
AI-assisted diagnosis
Automatic identification of endometrial lesions (accuracy 92%)
Bleeding risk prediction model (AUC=0.89)
New equipment
3D printing personalized mirror sheath
Self-expanding uterine cavity stent
Nanorobot targeted drug delivery

VII. Summary of clinical value
Modern hysteroscopy achieves:
Improved diagnostic accuracy: Early detection rate of endometrial cancer ↑60%
Reduced treatment trauma: 90% of surgeries are "day-to-day"
Protecting reproductive function: Pregnancy rate after adhesion lysis ↑35%
In the future, it will develop in the direction of intelligence, miniaturization, and integrated treatment, and it is expected to achieve the following within 5 years:
Outpatient hysteroscopy without anesthesia
Autologous cell regeneration and repair
Metaverse surgery teaching platform
Key data: The global hysteroscopy market size will reach $1.28 billion in 2023, with an annual growth rate of 8.7%
Faq
-
Does hysteroscopy require anesthesia?
Generally, there is no need for general anesthesia. Local anesthesia or intravenous analgesia can be used. The examination time is short, the patient has good tolerance, and postoperative observation takes 1-2 hours before leaving the hospital.
-
What gynecological diseases can hysteroscopy treat?
Suitable for the diagnosis and treatment of endometrial polyps, submucosal fibroids, intrauterine adhesions, etc. When combined with an electric cutting system, minimally invasive surgery can be performed to preserve fertility function.
-
What is the best time for hysteroscopy examination?
It is recommended to do it 3-7 days after the menstrual cycle is clean. At this time, the endometrium is thinner and the field of view is clearer, which can improve the accuracy of the examination and the safety of the surgery.
-
What should be noted after hysteroscopy surgery?
Two weeks after surgery, it is forbidden to take baths or engage in sexual activity, and vigorous exercise should be avoided. If there is fever, persistent abdominal pain, or abnormal bleeding, timely follow-up should be sought.
Latest articles
-
How XBX Cystoscope Supplier Ensures Quality and Precision for Hospital Procurement
Discover how the XBX Cystoscope Supplier provides hospitals with high-precision, OEM-ready endoscopy systems built for reliability, safety, and consistent imagi...
-
How XBX Bronchoscope Factory Delivers Reliable OEM Systems
Discover how the XBX Bronchoscope Factory ensures quality and reliability through advanced OEM manufacturing, optical precision, and strict quality control.
-
How XBX Laparoscope Minimizes Surgical Trauma in Abdominal Surgery
Discover how the XBX Laparoscope reduces surgical trauma through precision imaging, minimal incisions, and faster recovery in modern abdominal procedures.
-
How XBX Hysteroscope Detects and Removes Uterine Polyps
Discover how the XBX Hysteroscope enables precise detection and removal of uterine polyps, improving accuracy, safety, and comfort in women’s health care.
-
What Is an XBX Flexible Ureteroscope for Stone Removal?
Learn how the XBX flexible ureteroscope improves access, visibility, and efficiency in ureteral stone management with 4K imaging and ergonomic control.
Recommended products
-
Medical uroscope machine
Urological endoscopic examination is the gold standard for the diagnosis and treatment of urinary
-
Medical gastroscopy equipment
Medical gastroscopy equipment provides HD imaging for endoscopy medical endoscopes, enhancing diagno
-
XBX Repeating ENT Endoscope Equipment
Reusable ENT Endoscopes are medical optical instruments designed for examination of the ears, nose,
-
XBX Medical Repeating Bronchoscope
Reusable bronchoscope refers to a bronchoscope system that can be used multiple times after professi