ކޮންޓެންޓްސް ތާވަލް
އާތުރޮސްކޯޕީ އަކީ އާތުރޮސްކޯޕް ކިޔާ ތުނި، ކެމެރާ ޖަހާފައިވާ އާލާތެއް ބޭނުންކޮށްގެން ކަށީގެ ޑޮކްޓަރުންނަށް ސީދާ ހުޅުގެ އެތެރެއަށް ބަލާލެވޭ އެންމެ ކުޑަމިނުން އިންވޭސިވް ޕްރޮސީޖަރެކެވެ. އެއް ނުވަތަ އެއަށްވުރެ ގިނަ ކުދިކުދި އިންސިޝަންތަކުގެ ތެރެއިން ވައްދާފައިވާ މި ސްކޯޕުން ކާޓިލޭޖް، ލިގަމެންޓްސް، މެނިސްކީ، ސައިނޮވިއަމް އަދި އެހެނިހެން ސްޓްރަކްޗަރތަކުގެ ހައި ޑެފިނިޝަން ތަސްވީރުތައް މޮނިޓަރަކަށް ޕްރޮޖެކްޓް ކުރެއެވެ. ހަމަ މި ސެޝަންގައި ޚާއްޞަ މިނިއޭޗަރ އިންސްޓްރޫމެންޓްތަކުން މެނިސްކަލް ޓިއަރސް، ލުއި ހަށިގަނޑު، އިންފްލެމޭޑް ސައިނޯވިއަމް، ނުވަތަ ކާޓިލޭޖް ހަލާކުވުން ފަދަ މައްސަލަތައް ދެނެގަނެ ފަރުވާ ކުރެވިދާނެއެވެ. އޯޕަން ސާޖަރީއާ އަޅާބަލާއިރު، އާތުރޮސްކޯޕީގެ ސަބަބުން އާންމުކޮށް ރިހުން މަދުވެ، ކޮމްޕްލިކޭޝަންތައް މަދުވެ، ހޮސްޕިޓަލުގައި މަޑުކުރުން ކުރުވެ، ހަލުވިކަމާއެކު ރަނގަޅުވެ، ހުޅުގެ ޞައްޙަ، ރިއަލް ޓައިމް ވިޝުއަލައިޒޭޝަން ރައްކާތެރިވެއެވެ.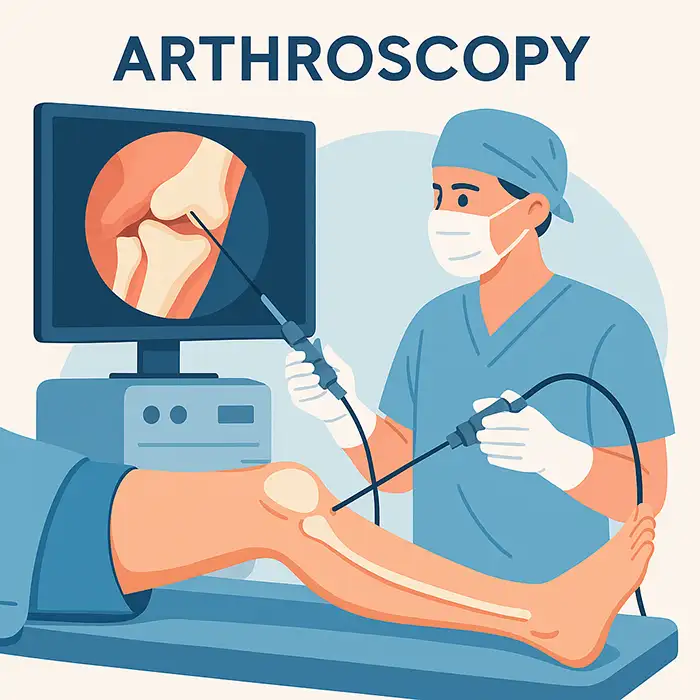
ގިނައިން “ޖޮއިންޓް އެންޑޯސްކޯޕީ” ގެ ނަމުން ނަންދެވިފައިވާ އާތުރޮސްކޯޕީ އަކީ ޑައިގްނޯސްޓިކް ޓެކްނިކެއްގެ ތެރެއިން އެންމެ ކުޑަމިނުން އިންވޭސިވް ފަރުވާ ދިނުމަށް ބޭނުންކުރާ ވަރސައިޓަލް ޕްލެޓްފޯމަކަށް ބަދަލުވި ކަމެކެވެ.
އެއީ ސްޕޯޓްސް މެޑިސިން އަދި ޖެނެރަލް އޯތޮޕެޑިކްސްގައި ކަކުލާއި ކޮނޑަށް އަދި އިތުރަށް އުނަގަނޑާއި ފައިގެ ކަކުލާއި އުނަގަނޑާއި އަތްތިލައަށް އާންމުކޮށް ކުރާ ކަމެކެވެ.
ކުދިކުދި ހަމުގެ އިންސިޝަންސް (ޕޯޓަލްސް) ގެ ސަބަބުން ޓިޝޫ ޓްރޮމާ، ސްކާރިންގ، އަދި މަސައްކަތުން ނުވަތަ ކުޅިވަރަކުން ދުރުހެލިވާ ވަގުތުތައް އޯޕަން އެޕްރޯޗްތަކާ އަޅާބަލާއިރު ކުޑަވެއެވެ.
އިންޓްރާ އާޓިކިއުލަރ ސްޓްރަކްޗަރސް ސީދާ ވިޝުއަލައިޒް ކުރުމުން އަލާމާތްތަކާއި އިމޭޖިންގ އިން ނިންމުމެއް ނެތް ވަގުތުތަކުގައި ސީދާ ޑައިގްނޯސިސް ކުރެވޭނެއެވެ.
އެއް ސެޝަންގައި ޑައިގްނޯސިސް އާއި ފަރުވާ އެއްކޮށްލައިގެން ޓޯޓަލް އެނެސްތެޝިއާ އަށް ހުށަހެޅޭ މީހުންނާއި ހަރަދު ކުޑަކުރެވިދާނެ އެވެ.
ސްޓޭންޑަރޑައިޒްޑް ޓެކްނިކްސް އަދި އިންސްޓްރޫމެންޓްސް އިން ފުޅާ ދާއިރާއެއްގައި ޕެތޮލޮޖީތަކުގެ ތެރެއިން ރިޕްރޮޑަކްޓިބަލް އައުޓްކަމްސް އަށް ސަޕޯޓް ކުރެއެވެ.
ފައިބަރ އޮޕްޓިކް ނުވަތަ އެލްއީޑީ އިލިމިނޭޝަން އާއި ހައި ޑެފިނިޝަން ޑިޖިޓަލް ކެމެރާ އާއި އެކު 4-6 އެމްއެމް ދިގުމިނުގެ ރިޖިޑް ނުވަތަ ސެމީ ފްލެކްސިބަލް ސްކޯޕެކެވެ.
އެއް ނުވަތަ އެއަށްވުރެ ގިނަ މަސައްކަތްކުރާ ޗެނަލްތަކުގެ ސަބަބުން ޝޭވަރސް، ގްރެސްޕަރސް، ޕަންޗްސް، ބާރސް، ރޭޑިއޯފްރީކުއެންސީ ޕްރޮބްސް، އަދި ސުޗުއަރ ޕާސިންގ ޓޫލްސް ފަދަ ތަކެތި ދަތުރުކުރެވޭނެއެވެ.
ފެންހިންދުމުގެ ނިޒާމަކުން ސްޓައިރިލް ސެލައިން ދައުރުކޮށް ޖޮއިންޓް ސްޕޭސް ފުޅާކޮށް، ކުނި ސާފުކޮށް، ވިޝުއަލައިޒޭޝަން ބެލެހެއްޓޭނެ އެވެ.
ތަސްވީރުތައް މޮނިޓަރެއްގައި ދައްކާއިރު ޓީމުން ނޭވިގޭޓްކޮށް މުހިއްމު ހޯދުންތައް ރެކޯޑް ކުރެ އެވެ.
ސްޓައިރިލް ޕްރެޕް އަދި ޑްރެޕިންގ އަށް ފަހު ޕޯޓަލްތައް އުފައްދަނީ ރައްކާތެރި އެނަޓޮމިކަލް ލޭންޑްމާކްތަކުގައި ބްލޭޑް ނުވަތަ ޓްރޯކާރ އެއް ބޭނުންކޮށްގެންނެވެ.
މި ސްކޯޕުން ކޮމްޕާރޓްމަންޓްތައް ނިޒާމީ ސިކުނޑިއެއްގެ ގޮތުގައި ސާވޭކޮށް، ކާޓިލޭޖް ސަރަހައްދުތަކާއި، ލިގަމެންޓްތަކާއި، ސައިނޮވިއަމް ލިޔެކިޔުންތައް ހުރެއެވެ.
ޕެތޮލޮޖީ ފެނިއްޖެނަމަ، އެކްސެސަރީ އިންސްޓްރޫމެންޓްތައް އިތުރު ޕޯޓަލްތަކުގެ ތެރެއިން ވަދެ، ޓިޝޫތައް ޑިބްރައިޑް، މަރާމާތު ނުވަތަ ރިކޮންސްޓްރަކްޓް ކުރެއެވެ.
ނިމުމުގައި ސެލައިން ހުސްކޮށް، ޕޯޓަލްތައް ސުޗުއަރ ނުވަތަ އެޑްހީޒިވް ސްޓްރިޕް ޖަހައިގެން ބަންދުކޮށް، ސްޓައިރިލް ޑްރެސިންގްސް ޖަހައެވެ.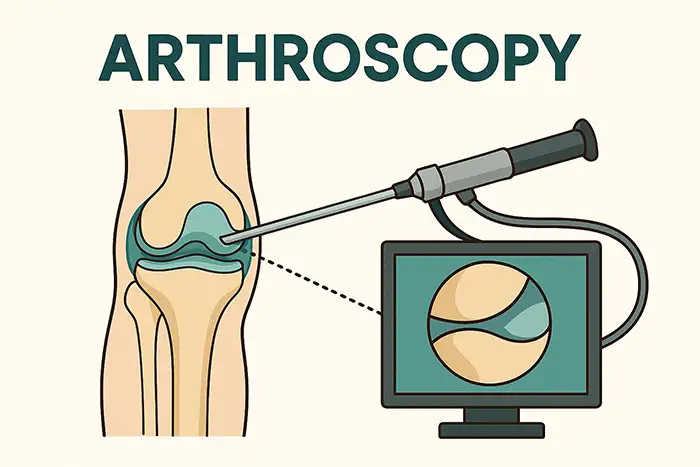
ކަކުލު ހުޅުގައި: މެނިސްކަލް ޓިއަރސް، ލުއި ހަށިގަނޑު، އެންޓިރިއަރ/ޕޮސްޓިރިއަރ ކްރޫޝިއޭޓް ލިގަމެންޓް އިންޖަރީ، ފޯކަލް ކާޓިލޭޖް ޑިފެކްޓްސް، ސައިނޮވައިޓިސް.
ކޮނޑުގައި: ރޮޓޭޓަރ ކަފް ޓިއަރސް، ލެބްރަލް ޓިއަރސް/އިންސްޓޭބިލިޓީ، ބައިސެޕްސް ޕެތޮލޮޖީ، ސަބްއެކްރޮމިއަލް އިމްޕިންގމަންޓް، އެޑްހީޒިވް ކެޕްސުލައިޓިސް ރިލީޒް.
ހީޕް/އެންކްލް/ރިސްޓް/އެލްބޯ: ފެމޯރޯއެސިޓެބިއުލަރ އިމްޕިންގމަންޓް، އޮސްޓިއޯކޮންޑްރަލް ލޭޝަންސް، ޓީއެފްސީސީ ޓިއަރސް، ލެޓަރަލް އެޕިކޮންޑައިލައިޓިސް ޑިބްރައިޑްމަންޓް.
ކްލިނިކަލް އިމްތިޙާނާއި އިމޭޖިންގ އެއްގޮތް ނުވާ ވަގުތުތަކުގައި ދިގުދެމިގެންދާ ހުޅުތަކުގައި ރިއްސުން ނުވަތަ ދުޅަވުމުގެ ޑައިގްނޯސްޓިކް އިވެލުއޭޝަން.
މެކޭނިކަލް އަލާމާތްތަކަށް އަވަހަށް ފަރުވާ ދިނުމުން ސެކަންޑަރީ ކާޓިލޭޖް ވޭއާ އާއި އޮސްޓިއޯއާތުރައިޓިސް އަށް ކުރިއެރުން ހުއްޓުވައެވެ.
ޓާގެޓްޑް ޑިބްރައިޑްމަންޓް ނުވަތަ ސްޓެބިލައިޒޭޝަން އަކީ ވާދަވެރި އެތުލީޓުންނަށް ރީއިންޖަރީގެ ނުރައްކާ ކުޑަކޮށްދޭ ކަމެކެވެ.
ސައިނޯވިއަމް ނުވަތަ ކާޓިލޭޖްގެ ބަޔޮޕްސީ އިން ބަލި ބަދަލުކުރާ ފަރުވާއަށް މަގުދައްކައިދިނުމަށްޓަކައި އިންފްލެމެޓަރީ ނުވަތަ އިންފެކްޝަސް އެޓިއޮލޮޖީސް ސާފުކޮށްދެއެވެ.
ތާރީޚާއި ޖިސްމާނީ ތަހުލީލުތަކުގައި ބޮޑަށް އަލިއަޅުވާލާފައިވަނީ ނުތަނަވަސްކަމާއި، ތަޅުލުމާއި، ދުޅަވުމާއި، ކުރިން ލިބުނު އަނިޔާތަކާއި ނުވަތަ ސާޖަރީތަކަށެވެ.
އިމޭޖިންގ ރިވިއު: އެލައިންމަންޓާއި ކަށިގަނޑަށް އެކްސްރޭ، މަޑު ޓިޝޫތަކަށް އެމްއާރުއައި/އަލްޓްރާސައުންޑް؛ ލެބްތަކުގައި ދައްކާފައިވާ ގޮތަށެވެ.
ބޭސް ދިނުމުގެ ޕްލޭން: އެންޓިކޮގްލިއުލެންޓްސް/އެންޓިޕްލެޓްލެޓްސް ވަގުތީ ގޮތުން އެޖެސްޓްކުރުން؛ އެލާޖީ އާއި އެނެސްތެޝިއާ ރިސްކް އެސެސްމަންޓް ހެދުން.
ރޯދަ ހިފުމުގެ އިރުޝާދުތައް އާންމުކޮށް ހޭނައްތާލުމުގެ 6-8 ގަޑިއިރު ކުރިން؛ ޕޯސްޓޮޕަރޭޓިވް ޓްރާންސްޕޯޓް ހަމަޖެއްސުން.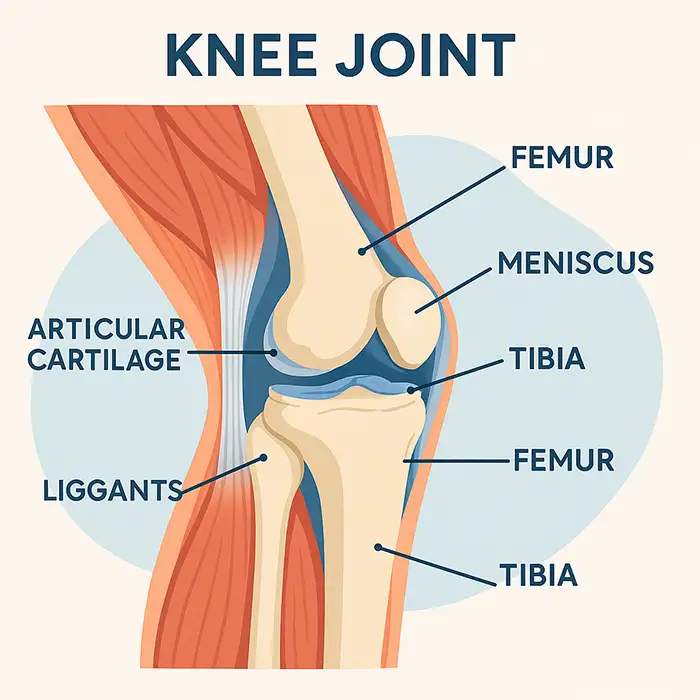
ޖޮއިންޓް، ޕްރޮސީޖަރ، އަދި ކޮމޮރބިޑިޓީސް އިން ހޮވާ ސެޑޭޝަން، ރީޖަނަލް ބްލޮކްސް، ސްޕައިނަލް، ނުވަތަ ޖެނެރަލް އެނެސްތެޝިއާ އާއި އެކު ލޯކަލް.
ފައިދާތަކާއި، ބަދަލުތަކާއި، ނުރައްކާތަކާއި، އޭގެ އިތުރުން މަސައްކަތާއި ކުޅިވަރަށް އެނބުރި އައުމަށް ޙަޤީޤީ ޓައިމްލައިންތަކާ ބެހޭގޮތުން މަޝްވަރާކުރުން.
އައިސިންގ، އެލެވޭޝަން، ޕްރޮޓެކްޓެޑް ބަރުދަން އުފުލުން، އަދި އިންޒާރުދޭ ނިޝާންތައް (ހުމުގެ އަސަރު، ރިހުން އިތުރުވުން، ކަކުލުގައި ދުޅަވުން) ދަސްކޮށްދިނުން.
ނާރުތަކާއި ހަންގަނޑު ރައްކާތެރިކުރުމަށްޓަކައި ޕެޑިންގ އާއި އެކު ޕޮޒިޝަން ކުރުން (އެބަހީ، ކަކުލު ހުޅުގައި ލެގް ހޯލްޑަރުގައި، ކޮނޑު ބީޗް-ޗެއާގައި ނުވަތަ ލެޓަރަލް ޑެކިއުބިޓަސްގައި) .
އެނަޓޮމިކަލް ލޭންޑްމާކްސް ފާހަގަކުރުން؛ ޖަރާސީމު ނެތް ހާލަތްތަކުގައި ވިއުވިންގ އަދި ވޯކިންގ ޕޯޓަލްތައް އުފެއްދުން.
ޑައިގްނޯސްޓިކް ސާރވޭ: ކާޓިލޭޖް ގްރޭޑްސް، މެނިސްކީ/ލެބްރަމް، ލިގަމެންޓްސް، ސައިނޮވިއަމް އިވެލުއޭޓްކުރުން؛ ފޮޓޯ/ވީޑިއޯ ކެޕްޗާރ ކުރުން.
ތެރަޕީ: ޕާރޝިއަލް މެނިސްސެކްޓޮމީ އާއި މަރާމާތުކުރުން، ރޮޓޭޓަރ ކަފް މަރާމާތުކުރުން، ލެބްރަލް ސްޓެބިލައިޒޭޝަން، މައިކްރޯފްރެކްޗަރ ނުވަތަ އޮސްޓިއޯކޮންޑްރަލް ގްރާފްޓިންގ.
ބަންދުކުރުން: ފްލޫޑް ނަގައި، ޕޯޓަލްތައް ބަންދުކޮށް، ކޮމްޕްރެސިވް ޑްރެސިންގ ޖަހައި، ޕޯސްޓޮޕަރޭޓިވް ޕްރޮޓޮކޯލް ވަގުތުން ފެށުން.
އެންމެ ކުޑަމިނުން އިންސިޝަން ޑިސްކޮމްފޯޓް؛ ގިނައީ ފުރަތަމަ 24-72 ގަޑިއިރު ތޫނު ރިހުން އަށްވުރެ ޕްރެޝަރު ނުވަތަ ހަރުވުން ސިފަކުރެއެވެ.
އެއްދުވަހަކު ޑިސްޗާޖް ވުމަކީ އާންމު ކަމެކެވެ؛ ރައްކާތެރިކަމަށްޓަކައި ކްރަޗް ނުވަތަ ސްލިންގް ބޭނުންވެދާނެއެވެ.
އެނަލްޖީޝިއާ އަކީ އެސިޓަމިނޯފެން/އެންއެސްއޭއައިޑީސް، ރީޖަނަލް ބްލޮކްސް، އަދި ބޭނުން ނަމަ ވަރުގަދަ އޭޖެންޓްތައް ކުރު މުއްދަތަކަށް ބޭނުންކުރުން އެއްކޮށްލާ އެއްޗެކެވެ.
ހަރުވުން ހަނިކުރުމަށާއި ކާޓިލޭޖްގެ ސިއްހަތު ކުރިއެރުވުމަށްޓަކައި އިރުޝާދު ދީފައިވާ ގޮތަށް އަވަހަށް ހަރަކާތްތެރިވުމަށް ހިތްވަރު ދެއެވެ.
އިންފެކްޝަން، ލޭއައުން، ޑީޕް ވެއިން ތްރޮމްބޮސިސް، ނާރު ނުވަތަ ލޭހޮޅިތަކަށް ރިއްސުން، އިންސްޓްރޫމެންޓް ފަޅައިގެން ދިއުން (މިހުރިހާ ކަމެއް ވެސް އާންމު ނޫން) އެވެ.
ދިގުދެމިގެންދާ ހަރުވުން ނުވަތަ ރިހުން ނުވަތަ ސްކާރިންގ ނުވަތަ އެޑްރެސް ނުކުރެވި ހުންނަ ޕެތޮލޮޖީގެ ސަބަބުން ރިއްސުން.
މަރާމާތު ނުކުރެވިއްޖެނަމަ (އެބަހީ، މެނިސްކަލް ނުވަތަ ރޮޓޭޓަރ ކަފް ރިޓިއަރ) ރިވިޝަން ސާޖަރީއެއް ހަދަންޖެހިގެން.
ސްޓްރިކްޓް ސްޓައިރިލް ޓެކްނިކް، އެންޓިބަޔޮޓިކް ޕްރޮފިލެކްސިސް އިންޑިކޭޓް ދިނުމާއި، ފަރުވާތެރިކަމާއެކު ޕޯޓަލް ބެހެއްޓުމެވެ.
ކޮންޓިނިއުއަލް ވިޝުއަލައިޒޭޝަން، ކޮންޓްރޯލްޑް ޕަމްޕް ޕްރެޝަރސް، އަދި މެޓިކިއުލަސް ހެމޮސްޓޭސިސް.
ކޮމްޕްލިކޭޝަންތައް އަވަހަށް ދެނެގަތުމާއެކު ސްޓޭންޑަރޑައިޒްޑް ރިހެބިލިޓޭޝަން މަގުތައް.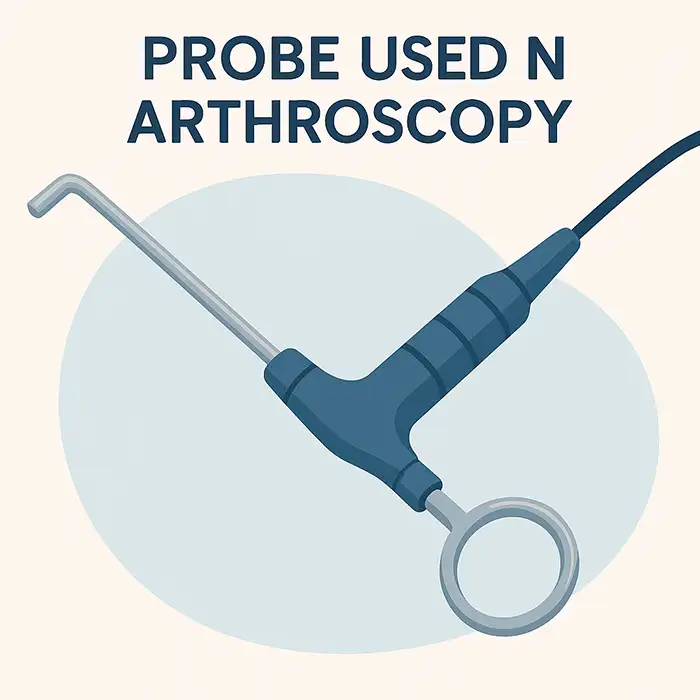
އެކްސްރޭ އިން ފެންނަނީ ފްރެކްޗަރސް އާއި އެލައިންމަންޓް ނަމަވެސް މަޑު ޓިޝޫތަކެއް ނޫނެވެ؛ އާތުރޮސްކޯޕީ އިން ސީދާ ކާޓިލޭޖް އަދި ލިގަމެންޓްސް އިންސްޕެކްޓް ކުރެއެވެ.
އެމްއާރުއައި އަކީ ނޮންއިންވޭސިވް އަދި ސްކްރީނިންގ އަށް މޮޅު އެއްޗެކެވެ؛ އާތުރޮސްކޯޕީ އިން ބޯޑަރލައިން ހޯދުންތައް ކަށަވަރުކޮށްދީ، އެކަމަށް ވަގުތުން ފަރުވާ ދެއެވެ.
އޯޕަން ސާޖަރީއާ އަޅާބަލާއިރު އާތުރޮސްކޯޕީ އިން ވެސް މިފަދަ ލަނޑުދަނޑިތައް ހާސިލް ކުރެވެނީ ކުދި އިންސިޝަންތަކެއް ޖަހައިގެން ހަރަކާތްތެރިކަމަށް އަވަހަށް އެނބުރި އައުމުންނެވެ.
އައިސް، ކޮމްޕްރެޝަން، އެލިވޭޝަން، އަދި އަމުރުކޮށްފައިވާ ގޮތަށް ޕްރޮޓެކްޓެޑް ވެއިޓް-ބެރިންގ ނުވަތަ ސްލިންގް އިމޮބިލައިޒޭޝަން.
ޒަޚަމްތަކަށް ފަރުވާ ދިނުން: 24-48 ގަޑިއިރު ވަންދެން ޑްރެސިންގްސް ހިކިކޮށް ބެހެއްޓުމާއި، ރަތްވުން ނުވަތަ ފެން ހިއްކުން މޮނިޓަރކުރުން.
ރެޕް އިން ކޮންޓްރެއިންޑިކޭޓް ނުކުރާހާ ހިނދަކު މަޑުމައިތިރި ރޭންޖް އޮފް މޯޝަން ކަސްރަތުތައް އަވަހަށް ފެށުން
އާތުރޮސްކޯޕީ އިން ވަނީ ޕްރިސިސް ވިޝުއަލައިޒޭޝަން އާއި މިނިމަލީ އިންވޭސިވް ޓްރީޓްމަންޓް އެއްކޮށްލައިގެން ޖޮއިންޓް ކެއާ ބަދަލުކޮށް، ކޮމްޕްލިކޭޝަންތައް މަދުވުމުން ބަލިމީހުން އަވަހަށް މަސައްކަތަށް އެނބުރި ކުޅިވަރަށް އައުމަށް އެހީތެރިވެދީފަ އެވެ. އޭގެ ސޭފްޓީ ޕްރޮފައިލް، ވަރސެޓިލިޓީ، އަދި ޓެކްނޮލޮޖީގެ ގޮތުން މެދުނުކެނޑި ކުރިއެރުން ލިބުމުން މިއީ ގިނަ ޖޮއިންޓް ޑިސްއޯޑަރސް އަށް ފުރަތަމަ ލައިން އޮޕްޝަނެކެވެ. އިތުބާރު ހުރި ހައްލުތައް ހޯދަން ބޭނުންވާ މުއައްސަސާތަކަށާއި ޑިސްޓްރިބިއުޓަރުންނަށް އިތުބާރު ހުރި ސަޕްލައިއަރަކާ ޕާޓްނަރޝިޕް ހެދުމަކީ ނަތީޖާތަކާއި އޮޕަރޭޝަނަލް އެފިޝަންސީ އިތުރުކޮށްދޭ ކަމެކެވެ. މަގު ނިމުމުން- ޑައިގްނޯސިސް އިން ފެށިގެން ރިކަވަރީއާ ހަމައަށް- ރަނގަޅަށް ހޮވާފައިވާ އިކުއިޕްމަންޓްތަކާއި ރަނގަޅަށް ތަމްރީނު ލިބިފައިވާ ޓީމުތަކުން ތަފާތު ގެނެސްދޭއިރު، އެކްސްބީއެކްސް ފަދަ ޕްރޮވައިޑަރުންނަށް ޒަމާނީ ސާޖިކަލް ސްޓޭންޑަޑްތަކަށް ފުރިހަމަ ސިސްޓަމްތަކާއި އިންސްޓްރޫމެންޓްތަކާއި ސަޕޯޓް ފޯރުކޮށްދެވިދާނެ އެވެ.
އާތުރޯސްކޯޕް އަކީ އާންމުކޮށް 4-6 އެމްއެމް ގެ ދިގުމިނުގެ ރިޖިޑް ސްކޯޕްތަކެއް ކަމަށާއި، މިއީ ކަކުލާއި، ކޮނޑާއި، އުނަގަނޑާއި، ފައިގެ ކަކުލާއި، އުނަގަނޑު ނުވަތަ އަތްތިލަ ފަދަ ކަންކަމަށް ފަރުމާކޮށްފައިވާ އެއްޗެކެވެ. ހޮސްޕިޓަލްތަކުން ކްލިނިކަލް ޑިމާންޑަށް ބަލައިގެން ޑައިގްނޯސްޓިކް ނުވަތަ ތެރަޕީޓިކް މޮޑެލްތައް ހޮވިދާނެ އެވެ.
ރެގިއުލޭޓަރީ ކޮމްޕްލައިންސް ކަށަވަރުކުރުމަށްޓަކައި ސަޕްލައި ކުރާ ފަރާތްތަކުން ސީއީ، އައިއެސްއޯ، ނުވަތަ އެފްޑީއޭ ސެޓްފިކެޓްތަކާއި، ސްޓިރިލައިޒޭޝަން ވެލިޑޭޝަން، އަދި ކޮލިޓީ އެޝުއަރެންސް ޑޮކިއުމަންޓޭޝަން ފޯރުކޮށްދޭންވާނެއެވެ.
ސްޓޭންޑަޑް ސެޓްތަކުގެ ތެރޭގައި ޝޭވަރސް، ގްރެސްޕަރސް، ޕަންޗްސް، ސުޗުއަރ ޕާސަރސް، ރޭޑިއޯފްރީކުއެންސީ ޕްރޮބްސް، އިރިގޭޝަން ޕަމްޕްސް، އަދި ޑިސްޕޯޒެބަލް ސްޓައިރިލް ކެނިއުލާސް ހިމެނެއެވެ.
އާދެ، މިޒަމާނުގެ އާތުރޮސްކޯޕީ ސިސްޓަމްތަކުގެ ސަބަބުން ސާޖަންންނަށް ހުޅުތަކުގެ ހާލަތު ދެނެގަނެ، މެނިސްކަސް މަރާމާތުކުރުމާއި، ލިގަމެންޓް ރިކޮންސްޓްރަކްޝަން ނުވަތަ ކާޓިލޭޖް ފަރުވާ ފަދަ ކަންކަން ވަގުތުން ކުރެވޭނެއެވެ.
ހައި ޑެފިނިޝަން ޑިޖިޓަލް ކެމެރާތަކާއި، އެލްއީޑީ އަލިކުރުމާއި، ރެކޯޑިން ކެޕޭސިޓީއާއި، ހޮސްޕިޓަލް ޕެކްސް ސިސްޓަމްތަކާ އެއްގޮތްވުމަކީ ކްލިނިކަލް ބޭނުންތަކަށް މުހިންމު ސިފަތަކެކެވެ.
އާންމުކޮށް ސަޕްލައި ކުރާ ފަރާތްތަކުން 1-3 އަހަރުގެ ވޮރެންޓީ، ޕްރިވެންޓިވް މެއިންޓެނަންސް، ސޮފްޓްވެއާ އަޕްގްރޭޑް، އަދި ޓްރެއިނިންގ އޮޕްޝަންތަކާއެކު ޓެކްނިކަލް ސަޕޯޓް ފޯރުކޮށްދެއެވެ.
އާދެ، ގިނަ ސަޕްލައި ކުރާ ފަރާތްތަކުގެ ތެރޭގައި އޮންސައިޓް ޓްރެއިނިންގ، ޑިޖިޓަލް ޓިއުޓޯރިއަލް، އަދި ސާޖަން އާއި މުވައްޒަފުންނަށް އިކުއިޕްމަންޓް އޮޕަރޭޝަން އަށް އިތުބާރު ކުރެވޭތޯ ބެލުމަށް ޓެކްނިކަލް ސަޕޯޓް ހިމެނެއެވެ.
އިކުއިޕްމަންޓްތައް ކޮންޓްރޯލްޑް ޕަމްޕް ޕްރެޝަރާއި، ސާފު ވިޝުއަލައިޒޭޝަން އާއި، ސްޓައިރިލް ޕްރޮޓޮކޯލްތަކަށް ސަޕޯޓް ކުރަން ޖެހެއެވެ. އަދި ކުއްލި ހާލަތުގައި ދިމާވާ މައްސަލަތައް ހައްލުކުރުމާ ބެހޭ ގޮތުން ވެސް ސަޕްލައި ކުރާ ފަރާތްތަކުން އިރުޝާދު ދޭން ޖެހެ އެވެ.
ޕްރޮކިއުމަންޓް ޓީމުތަކުން ސްޕެސިފިކޭޝަންތަކާއި، ސާވިސް ޕެކޭޖްތަކާއި، ޓްރޭނިންގ ސަޕޯޓާއި، ވޮރެންޓީ ޓާމްސް އަޅާކިޔައި، ސާބިތު ކްލިނިކަލް ތަޖުރިބާއާއި ސޭލްސްއަށްފަހު އިތުބާރު ކުރެވޭ ސަޕްލައިއަރުން ހޮވަންވާނެއެވެ.
އާދެ، ގިނަ ނިޒާމުތަކަކީ މޮޑިއުލާ ނިޒާމުތަކެއް ކަމުން، ހުޅުތަކަށް ޚާއްޞަ އިންސްޓްރޫމެންޓްތަކާއެކު ކަކުލާއި ކޮނޑާއި އުނަގަނޑާއި ނުވަތަ ފައިގެ ކަކުލުގެ ޕްރޮސީޖަރސް ހުރަސްކޮށް އެއް ކެމެރާއާއި އަލި ސޯސްއެއް ބޭނުންކުރެވޭނެއެވެ.
ކޮޕީރައިޓް © 2025.ގީކްވެލިއު ހުރިހާ ހައްޤުތަކެއް ލިބިގެންވެއެވެ.ޓެކްނިކަލް ސަޕޯޓް: TiaoQingCMS