Table of Contents
Laryngoscopy is a medical procedure that allows doctors to examine the larynx, including the vocal cords and surrounding structures, using a device called a laryngoscope. It is performed to diagnose throat disorders, evaluate airway function, and guide treatments such as intubation or biopsy, making it an essential tool in modern clinical practice.
Laryngoscopy is a medical examination that allows clinicians to visualize the larynx, vocal folds, and adjacent structures with a laryngoscope to diagnose disease, secure the airway, and guide treatment. In practice, the technique spans routine clinic assessments and life-saving interventions in anesthesia and emergency care. Understanding what laryngoscopy is, how each approach differs, and where it fits in modern care helps patients and professionals make safer, better-informed decisions.
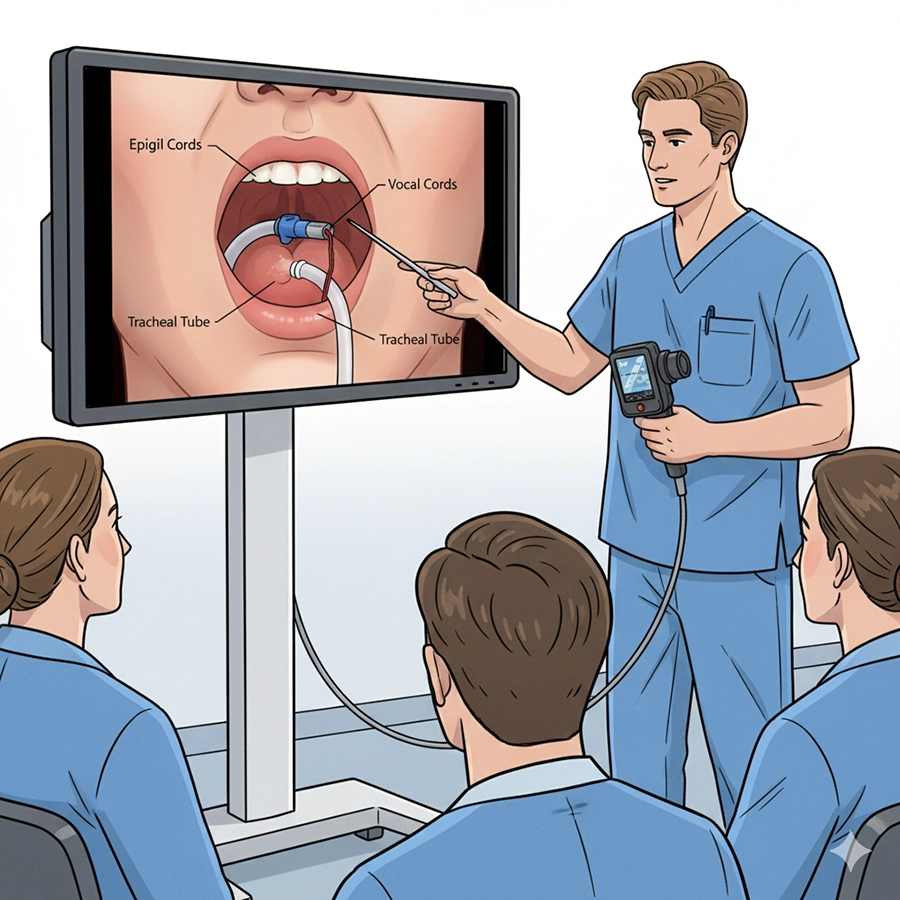
Laryngoscopy is defined as the direct or indirect visualization of the larynx and vocal folds using a rigid or flexible scope, sometimes with video enhancement. For those asking what is laryngoscopy, the essential answer is that it provides clinicians with a clear look at the structures responsible for voice production and airway protection. A typical laryngoscopy definition emphasizes both diagnostic and therapeutic use: identifying abnormalities such as nodules or tumors and enabling interventions like endotracheal intubation or biopsy.
The basic equipment includes a handle, a blade, and a light source. Modern designs integrate fiber-optic illumination or digital cameras for improved imaging. The procedure overcomes the natural curvature of the airway, allowing clinicians to align their view with the glottic opening. Depending on the purpose, laryngoscopy may be performed in outpatient clinics, operating rooms, or intensive care units. Indications include hoarseness, persistent sore throat, difficulty breathing, suspected laryngeal cancer, or airway trauma.
In anesthesia, a laryngoscopy procedure is performed before many surgeries to insert a breathing tube. This step protects the lungs, ensures ventilation, and allows safe delivery of anesthetic gases. In critical care, securing an airway with laryngoscopy is often the difference between life and death in emergencies such as respiratory failure. Preparation is crucial: patients may receive topical anesthesia, decongestants for nasal routes in flexible laryngoscopy, and careful positioning to optimize the view. Risks are low but include sore throat, bleeding, or rare complications like laryngospasm.
Laryngoscopy definition: visualization of the larynx for diagnosis and treatment.
Equipment has evolved from simple blades to high-definition video systems.
Indications include diagnostic evaluation, intubation, and biopsy.
Risks are minimal when performed by trained professionals.
Several types of laryngoscopy have been developed, each designed for specific clinical goals.
Direct laryngoscopy uses a rigid blade to align oral, pharyngeal, and laryngeal axes, providing a direct line of sight. It is fast, widely available, and most often used for intubation. Its limitation is reduced visibility in difficult airway situations.
Video laryngoscopy employs a miniature camera on the blade tip, transmitting the view to a screen. This technique improves visualization, especially in challenging airways, and allows the entire medical team to observe. It is more expensive but valuable for training and patient safety.
Flexible laryngoscopy involves a slender, steerable fiber-optic or digital scope inserted through the nose or mouth. It enables dynamic assessment of vocal cords during breathing or speaking and is commonly used in ENT clinics. It is less suited for emergency intubations but excellent for diagnostics.
Rigid laryngoscopy provides a magnified and stable view for surgical precision. ENT surgeons use it under anesthesia for biopsies, tumor removal, or laser procedures. It offers superior brightness and stability but requires operating-room resources.
| Type of Laryngoscopy | Visualization | Strengths | Limitations | Common Uses |
|---|---|---|---|---|
| Direct Laryngoscopy | Line-of-sight | Fast, simple, low cost | Limited in difficult airways | Routine intubation, emergencies |
| Video Laryngoscopy | Screen display | Enhanced view, team teaching | Higher cost, needs power | Difficult airway, training |
| Flexible Laryngoscopy | Dynamic nasal/oral scope | Awake diagnostics, voice evaluation | Not suitable for emergencies | ENT clinic, outpatient |
| Rigid Laryngoscopy | Magnified surgical view | Precise, bright image | Requires anesthesia | ENT surgery, biopsy |
 Pros and Cons Summary
Pros and Cons SummaryDirect: efficient and reliable, but challenging in complex anatomy.
Video: excellent visualization, higher cost.
Flexible: comfortable for patients, great for diagnostics.
Rigid: precise for surgery, resource-intensive.
A laryngoscopy procedure follows structured steps: assessment, preparation, visualization, and intervention. Doctors assess symptoms, airway anatomy, and risk factors. Preparation varies: topical anesthetic for flexible scopes, preoxygenation for intubation, and positioning to maximize oxygen reserve. Visualization requires steady insertion and often external manipulation to improve the view. Interventions may include intubation, biopsy, or removal of lesions.
Applications are wide-ranging. In airway management, laryngoscopy ensures safe intubation during surgery or emergencies. In ENT diagnostics, flexible scopes reveal vocal cord motion, tumors, or inflammation. In surgical uses, rigid scopes allow removal of foreign bodies, excision of growths, or precise laser treatments. For education, video laryngoscopy has transformed teaching, enabling trainees and supervisors to share the same view and review recordings.
Complications are rare but include sore throat, bleeding, or trauma. Proper preparation and technique minimize risks. Rescue strategies and adherence to airway management algorithms further enhance safety.
Persistent hoarseness or unexplained throat symptoms.
Suspected laryngeal cancer or lesions.
Emergency airway management.
Preoperative assessment and intubation.
Laryngoscopy is central to modern healthcare because it combines diagnostic precision with therapeutic capability. It allows early detection of laryngeal cancer, reducing delays in treatment. It ensures safe anesthesia by providing reliable airway access. It helps diagnose functional voice disorders and supports speech therapy planning.
From a systems perspective, video laryngoscopy improves consistency and training, allowing supervisors and trainees to share live views. For patients, flexible laryngoscopy is usually quick and minimally uncomfortable, offering immediate results without general anesthesia. Infection control has advanced with single-use blades and validated sterilization protocols, ensuring patient safety.
Economically, the benefits outweigh costs by reducing failed intubations, shortening surgery time, and improving diagnostic efficiency. Multidisciplinary collaboration is also enhanced, as ENT specialists, anesthetists, pulmonologists, and speech-language therapists all rely on laryngoscopic findings for joint decision-making.
Patients with airway or voice disorders.
Surgical and ICU patients needing intubation.
Medical trainees learning airway skills.
Hospitals prioritizing safety and infection control.
Technological innovation continues to transform laryngoscopy. High-definition and 4K video laryngoscopes provide superior clarity. Disposable scopes and blades improve infection control. AI-assisted visualization is emerging, with algorithms that may highlight anatomical landmarks or quantify vocal cord motion. Wireless and portable laryngoscopes extend access to remote or emergency settings.
Training has also evolved: simulation labs replicate airway challenges, allowing doctors to practice with direct, video, and flexible laryngoscopy. Integration with electronic medical records enables automated documentation, image storage, and remote consultation. Future developments may include multimodal imaging that combines light and ultrasound for improved diagnostic accuracy.
Expansion of AI in diagnosis and training.
Increased adoption of single-use flexible scopes.
Wider integration with digital health records.
Portable and wireless designs for field use.
Laryngoscopy unites diagnosis, airway safety, and surgical precision. Whether through direct laryngoscopy for rapid intubation, video laryngoscopy for teaching and safety, or flexible laryngoscopy for outpatient diagnostics, the procedure remains indispensable. With ongoing advances in imaging, infection control, and digital integration, laryngoscopy will continue to play a vital role in patient care across disciplines.
The laryngoscope does not exist in isolation; it is one of several key devices within the broader field of endoscopy. Modern clinical practice increasingly emphasizes integration, where the laryngoscope works alongside other specialized endoscopes to provide comprehensive visualization of the upper airway, gastrointestinal tract, urinary system, and more. By understanding how the laryngoscope complements these devices, clinicians can design diagnostic and therapeutic strategies that are safer, more efficient, and more effective for patients.
The bronchoscope and the laryngoscope share a natural relationship, as both devices are dedicated to airway management. While the laryngoscope primarily provides access to the larynx and vocal cords, the bronchoscope extends further into the trachea and bronchial tree. In a clinical setting, the laryngoscope is often the first tool used to visualize the glottic opening, making it easier to introduce a bronchoscope safely into the trachea. This complementary sequence is especially useful in patients with suspected airway obstruction or when managing complex intubations.
Flexible bronchoscopes are frequently introduced under direct laryngoscopic guidance, reducing the risk of trauma to delicate laryngeal structures. Video laryngoscopes also allow the simultaneous viewing of the glottis by the anesthesiologist and the bronchoscopist, improving teamwork during critical procedures. In research and teaching, this pairing provides trainees with a layered understanding of the upper and lower airways, reinforcing the importance of stepwise visualization.
The larynx and the esophagus are anatomically adjacent, which means that laryngoscopes and esophagoscopes are often used in tandem. When evaluating dysphagia, aspiration, or suspected lesions at the hypopharyngeal-esophageal junction, the laryngoscope allows initial inspection of the vocal cords and arytenoids, while the esophagoscope continues the examination into the esophagus. This dual approach helps physicians determine whether swallowing problems originate from vocal cord dysfunction, structural narrowing, or esophageal motility disorders.
Rigid esophagoscopes historically required laryngoscopic exposure for safe introduction. Even today, flexible esophagoscopes benefit from laryngoscopic assistance in patients with challenging anatomy. This interdependence highlights how the laryngoscope functions not only as a diagnostic tool but also as a gateway for introducing adjacent endoscopic devices into deeper structures.
The nasopharyngoscope provides detailed views of the nasal passages and nasopharynx, while the laryngoscope specializes in direct access to the larynx. In conditions such as obstructive sleep apnea, chronic sinusitis with laryngeal involvement, or vocal resonance disorders, both instruments are valuable. The nasopharyngoscope can trace airflow pathways from the nasal cavity to the oropharynx, and the laryngoscope completes the picture by capturing vocal cord function. When used together, these endoscopes allow clinicians to evaluate the entire upper airway as a functional unit rather than as isolated segments.
This holistic assessment is particularly important in pediatric care, where airway compromise may involve both adenoidal hypertrophy and laryngeal collapse. Coordinated use of nasopharyngoscopy and laryngoscopy improves diagnostic accuracy and helps determine whether surgical intervention, such as adenoidectomy or supraglottoplasty, is indicated.
Although the laryngoscope and gastroscope target distinct organ systems, they often converge in the evaluation of symptoms like chronic cough, reflux, and throat irritation. The laryngoscope allows the clinician to detect laryngeal inflammation or vocal cord lesions potentially caused by laryngopharyngeal reflux, while the gastroscope assesses the esophagus, stomach, and duodenum for evidence of gastroesophageal reflux disease. This complementary approach is critical because symptoms alone rarely distinguish airway irritation from digestive pathology.
By combining findings from both devices, physicians can provide more precise diagnoses and tailor treatment strategies. For example, visible laryngeal edema under the laryngoscope combined with esophagitis detected by gastroscopy strengthens the case for aggressive reflux management. Without this dual assessment, patients might receive incomplete or misleading advice.
Although the laryngoscope and cystoscope serve entirely different anatomical systems—the larynx and the bladder—they share technological and procedural parallels. Both devices rely on rigid and flexible designs, light transmission, and image capture technologies. Innovations pioneered in laryngoscopy, such as high-definition video and disposable blades, often inspire adaptations in cystoscopic design. Likewise, advances in irrigation systems and working channels from urology have informed certain laryngoscopic interventions, such as suctioning or laser fiber delivery.
This cross-pollination of endoscopic technologies underscores how the laryngoscope fits into a broader continuum of minimally invasive tools. Hospitals that invest in high-quality endoscopic imaging platforms often benefit from equipment standardization across departments, reducing training time and streamlining maintenance.
The arthroscope, designed for joint inspection, may seem far removed from airway visualization, but both devices exemplify the versatility of endoscopic technology. Miniaturization, optical clarity, and ergonomic handle design are engineering challenges faced by both arthroscope and laryngoscope manufacturers. As a result, innovations in one area frequently influence the other. For example, lightweight fiberoptic bundles developed for laryngoscopes have been adapted for arthroscopes, while improved irrigation systems in arthroscopy have inspired better suction mechanisms for laryngeal surgery.
These shared engineering principles emphasize that the laryngoscope is not an isolated tool but part of a multidisciplinary ecosystem where technical progress in one domain accelerates progress in others.
From a practical standpoint, the laryngoscope complements other endoscopes through its role in operating room workflows. For anesthesiologists, it is the device of choice for securing the airway prior to procedures involving the bronchoscope, gastroscope, or esophagoscope. For otolaryngologists, it provides the initial visualization required before transitioning to more specialized scopes. This layered usage prevents duplication of effort and ensures that each instrument is applied where it performs best.
Video integration platforms further enhance this collaboration. Modern operating theaters feature centralized screens where images from the laryngoscope, bronchoscope, and gastroscope can be displayed side by side. Such integration improves multidisciplinary communication, as surgeons, anesthesiologists, and gastroenterologists can simultaneously interpret findings and adjust strategies in real time.
Looking forward, the boundaries between different endoscopes are becoming increasingly fluid. Hybrid devices that combine laryngoscopic and bronchoscopic functions are under development, enabling seamless transition from the vocal cords to the lower airway. Similarly, multi-port platforms may allow clinicians to switch between laryngoscopic and esophagoscopic views without removing the device. These innovations aim to reduce procedure time, limit patient discomfort, and expand diagnostic accuracy.
Artificial intelligence is another area where the laryngoscope will complement other systems. Algorithms trained on large datasets of endoscopic images can simultaneously analyze laryngoscopic and gastroscopic findings, flagging subtle abnormalities that might be overlooked by the human eye. The result is a future where endoscopes are not only complementary in function but also interconnected through intelligent data sharing.
For medical trainees, understanding the complementary roles of endoscopes fosters a systems-based approach to patient care. Simulation labs now feature integrated mannequins that allow practice with laryngoscopes, bronchoscopes, and nasopharyngoscopes in a single session. This holistic training environment reinforces the idea that airway and digestive tract management are interconnected, and that proficiency with one scope supports proficiency with another. Such cross-training is vital in emergency settings where clinicians must quickly determine which device is most appropriate for a given situation.
Ultimately, the integration of the laryngoscope with other endoscopic systems serves one goal: improving patient outcomes. Coordinated use of devices reduces the need for multiple separate procedures, minimizing anesthesia exposure and recovery time. It also enhances diagnostic accuracy, ensuring that conditions involving overlapping anatomical regions are fully understood. For patients, this translates to faster diagnoses, less discomfort, and more targeted therapies.
In conclusion, the laryngoscope is best understood not as a standalone device but as a cornerstone of an interconnected endoscopic ecosystem. By complementing bronchoscopes, esophagoscopes, nasopharyngoscopes, gastroscopes, cystoscopes, and arthroscopes, it ensures comprehensive visualization across multiple anatomical systems. The result is a practice of medicine that is more precise, collaborative, and responsive to the complex needs of patients.
Direct laryngoscopy requires a straight line of sight to the vocal cords, while video laryngoscopy uses a camera and monitor, offering better visualization in difficult airway cases.
Flexible laryngoscopy can be performed under topical anesthesia, provides real-time evaluation of vocal cord motion, and causes minimal discomfort, making it ideal for outpatient diagnostics.
Hospitals should confirm compliance with ISO, CE, and FDA standards to ensure safety, performance, and international acceptance of laryngoscopy devices.
Single-use blades reduce infection risks and save sterilization costs, while reusable blades are more economical long-term. The choice depends on hospital policies and patient volume.
Laryngoscopy procedures in critical care focus on securing the airway, diagnosing airway obstructions, and assisting in emergency intubations under controlled visualization.
Video laryngoscopy allows trainees and supervisors to share the same view on a monitor, improving teaching efficiency, feedback, and patient safety.
Risks include sore throat, minor bleeding, dental trauma, or rare complications like laryngospasm. With proper preparation and skilled operators, complications are uncommon.
Evaluation should include upfront equipment cost, durability, training requirements, maintenance, and long-term savings from reduced complications and improved patient safety.
Advances include high-definition and 4K video, portable and wireless devices, AI-assisted visualization, and increased adoption of disposable flexible scopes for infection control.
Rigid laryngoscopy provides a stable, magnified view, making it the preferred choice for surgical precision in biopsies, tumor excision, and laser procedures.
Copyright © 2025.Geekvalue All rights reserved.Technical Support:TiaoQingCMS