Table of Contents
A medical endoscope works by transmitting light and images through a flexible or rigid tube that is inserted into the body, allowing doctors to view internal organs and tissues without major surgery. The scope integrates a light source, imaging system, and instrument channels, enabling both diagnostic and therapeutic procedures in real time.
Medical endoscopes have transformed modern healthcare by enabling minimally invasive examinations and treatments. Instead of relying on large incisions, physicians can use an endoscope to directly visualize internal organs and pathways such as the gastrointestinal tract, lungs, urinary system, and joints. This ability to see inside the body without surgery not only improves diagnostic accuracy but also reduces patient recovery time and hospital costs.
The application of medical endoscopes spans across multiple specialties. Gastroenterologists use them to perform colonoscopy and gastroscopy; pulmonologists rely on bronchoscopes to inspect the airways; urologists adopt cystoscopes and ureteroscopes to access the urinary tract; and surgeons utilize laparoscopes and arthroscopes for minimally invasive operations. This wide range of applications demonstrates how essential endoscopes have become in modern medicine.
To understand how medical endoscopes work, it is important to break down their core components. Although different models may vary in design, they share a similar architecture that includes the following parts:
LED Technology: Modern endoscopes primarily use LED illumination because it is energy efficient, produces bright white light, and generates less heat.
Fiber Optic Transmission: In older systems, fiber optic bundles transmit light from an external source to the end of the insertion tube.
Optical Lenses: Traditional endoscopes relied on rod-lens systems to carry images back to the eyepiece.
Digital Sensors: Current designs integrate CMOS or CCD sensors at the tip of the scope, transmitting high-resolution video to external monitors.
Flexible Tubes: Built with bendable materials, they allow navigation through the curves of the gastrointestinal tract or bronchial tree.
Rigid Tubes: Made from stainless steel or similar materials, they provide stability for procedures such as laparoscopy or arthroscopy.
The control handle allows the operator to steer the tip of the scope, adjust focus, and manage suction or irrigation. Buttons and knobs are ergonomically placed to minimize fatigue during long procedures.
One of the most valuable features of an endoscope is its working channel. This narrow pathway allows insertion of biopsy forceps, snares, scissors, or suction catheters, enabling therapeutic actions in addition to visualization.
The working principle of a medical endoscope can be summarized as a step-by-step process that integrates illumination, visualization, and intervention:
A powerful light is transmitted to the tip of the scope, illuminating the internal cavity. Adequate lighting is critical because internal organs are naturally dark and cannot be observed without artificial illumination.
The illuminated tissue is captured by either a lens system or a digital camera sensor. The images are then transmitted through fiber optics or electronic signals to an external monitor where the physician can view real-time video.
The working channel of the scope provides access for surgical instruments. Biopsies can be taken by inserting forceps through the channel, or bleeding can be controlled using cautery probes. This dual diagnostic and therapeutic capability is what makes endoscopy so versatile.
Endoscopes are also equipped with suction ports to remove fluids, mucus, or blood. Irrigation systems allow flushing of the field of view, ensuring that the physician has a clear perspective during the procedure.
In gastrointestinal endoscopy, air or carbon dioxide insufflation is used to expand the lumen, making it easier to navigate the scope and visualize structures. Carbon dioxide is preferred because it is absorbed more quickly and reduces patient discomfort.
The captured images are displayed on high-definition monitors. Physicians can record these videos for documentation, training, or post-procedure analysis. Advanced systems also allow for image enhancement using filters and AI-based diagnostic tools.
Medical endoscopes are designed in different forms depending on their intended application. Understanding the types of endoscopes helps illustrate how they work in various medical specialties.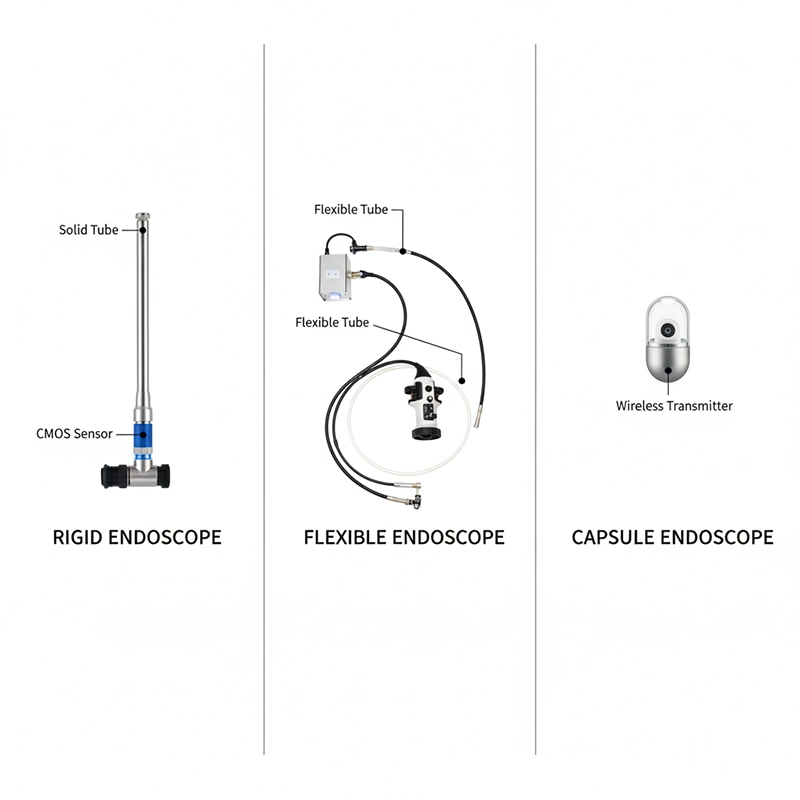
Laparoscopes: Used in abdominal and pelvic surgery, they provide stable, high-resolution images for minimally invasive operations.
Arthroscopes: Designed for joint inspection and repair, especially in the knee, shoulder, or hip.
Cystoscopes: Used by urologists to view the bladder and urinary tract with precise control.
Gastroscopes: Thin, flexible tubes used for esophagus and stomach visualization.
Colonscopes: Longer scopes for large intestine examination and polyp removal.
Bronchoscopes: Designed to enter the respiratory tract and assess airway conditions.
Capsule endoscopy is a non-invasive method where the patient swallows a pill-sized camera that captures images of the gastrointestinal tract. The images are transmitted wirelessly to an external receiver, offering visualization of areas difficult to reach with conventional scopes.
Traditional fiber-optic endoscopes rely on bundles of glass fibers to transmit images, while modern video endoscopes use digital chip-on-tip technology, which provides higher resolution and advanced imaging features.
The clarity of images produced by an endoscope is critical for accurate diagnosis. Several innovations have improved imaging over time:
Fiber optic systems deliver acceptable resolution but are limited by distortion and fragility. Digital sensors such as CCD and CMOS provide high-definition video and are now standard in advanced systems.
Modern medical endoscopes are equipped with HD and even 4K imaging capabilities, enabling clinicians to detect subtle lesions, small polyps, or microvascular changes that could be missed with lower resolution.
Narrow Band Imaging (NBI): Uses filtered light to highlight blood vessels and mucosal structures.
Fluorescence Imaging: Employs special dyes and light to identify abnormal tissues.
AI-Assisted Imaging: Artificial intelligence algorithms help flag suspicious lesions in real time.
Light delivery has evolved significantly in medical endoscopes:
Halogen and Xenon: Older light sources, powerful but inefficient and heat-producing.
LED: Now the preferred option for efficiency, long lifespan, and cooler operation.
Fiber Optics: Still used in some scopes to transmit light, though being replaced by direct LED illumination.
Safety is a key aspect of how medical endoscopes work. Infection prevention and patient comfort are priorities in design and usage.
Reusable endoscopes require high-level disinfection after each procedure. Automated reprocessing machines and single-use disposable scopes are gaining popularity to reduce cross-contamination risks.
Design improvements reduce strain on physicians’ hands and wrists, lowering the risk of repetitive stress injuries during long procedures.
Flexible scopes now use biocompatible, lightweight materials that balance durability with patient comfort, reducing the risk of trauma during insertion.
The working principle of medical endoscopes translates into a wide range of clinical applications:
Colonoscopy: Screening for colorectal cancer, polyp removal, bleeding control.
Gastroscopy: Evaluation of ulcers, reflux disease, and upper GI tumors.
Bronchoscopy: Used to examine the trachea and lungs, remove foreign bodies, or perform biopsy.
Cystoscopy: Visualization of the bladder for stones, tumors, or infections.
Ureteroscopy: Inspection of ureters and kidneys, often used for stone retrieval.
Laparoscopy: Abdominal procedures including gallbladder removal or gynecologic surgery.
Arthroscopy: Joint repair with minimal incision.
Rhinoscopy: Inspection of nasal passages for obstruction or infection.
Laryngoscopy: Examination of vocal cords and throat lesions.
The price of medical endoscopes depends on technology, specialty, and brand. Entry-level flexible scopes may cost several thousand dollars, while high-definition video systems with processors and monitors can exceed tens of thousands. Disposable scopes offer predictable per-use costs but increase overall expenditure when used frequently.
Market insights reveal steady growth in the endoscopy segment, driven by rising demand for minimally invasive procedures, improved imaging, and infection prevention technologies. Hospitals and clinics evaluating how medical endoscopes work in practice often factor in not only performance but also maintenance and training costs.
For B2B buyers, selecting the right endoscope requires balancing clinical requirements, budget, and supplier reliability. Key considerations include:
Matching scope type to medical specialty
Comparing suppliers and warranty terms
Evaluating training and technical support services
Considering future compatibility with imaging upgrades
Light Sources: High-efficiency LEDs and xenon lamps for optimal illumination.
Processors: Units that enhance image quality and integrate with hospital IT systems.
Monitors: High-resolution screens for real-time guidance during procedures.
Recording Systems: Tools for documentation, teaching, and post-procedure analysis.
The future of how medical endoscopes work is moving toward greater integration with AI, robotics, and miniaturized imaging. Disposable scopes are expected to reduce infection risks, while robotic-assisted systems may enhance precision during complex surgeries. Advances in imaging, including 3D visualization and augmented reality, are also shaping the next generation of devices.
These innovations demonstrate that medical endoscopes will continue to play a central role in diagnostics and therapy, offering clinicians safer, more efficient, and more accurate tools to care for patients.
A medical endoscope is a diagnostic and surgical instrument that uses a thin, flexible or rigid tube with a light source and camera to view internal organs without large incisions.
Medical endoscopes work by transmitting light into the body, capturing images with a lens or digital sensor, and displaying real-time video on a monitor. Many models also have working channels for instruments, suction, or irrigation.
The main types include rigid endoscopes (laparoscope, arthroscope), flexible endoscopes (gastroscope, colonoscope, bronchoscope), and capsule endoscopes, which use a swallowable camera pill.
Medical endoscopes are used in colonoscopy, gastroscopy, bronchoscopy, cystoscopy, laparoscopy, arthroscopy, and ENT examinations, covering multiple specialties.
Yes, when properly sterilized or used as disposable models, medical endoscopes are safe. Modern designs also improve ergonomics, minimize patient discomfort, and reduce infection risks.
Copyright © 2025.Geekvalue All rights reserved.Technical Support:TiaoQingCMS