Table of Contents
In 2025, colonoscope prices range between $8,000 and $35,000, depending on technology level, manufacturer, and procurement strategies. Entry-level HD models remain affordable for smaller clinics, while advanced 4K and AI-assisted systems are priced at the upper end, reflecting the premium associated with innovation. Disposable colonoscopes, although not widely adopted in all regions, introduce a new pricing model based on per-procedure costs. Beyond the device itself, hospitals must also account for processors, monitors, sterilization equipment, training, and ongoing service contracts. Understanding these factors is critical for procurement teams, as colonoscope purchases represent a substantial portion of diagnostic capital expenditure in gastroenterology.
The colonoscope market in 2025 reflects global healthcare priorities. Rising awareness of colorectal cancer, identified by the World Health Organization (WHO) as the second leading cause of cancer-related deaths worldwide, is driving governments to expand national screening programs. This creates consistent demand for colonoscopy systems in both developed and developing countries. According to Statista, the global endoscopy equipment market is projected to exceed USD 45 billion by 2030, with colonoscopes accounting for a significant share of diagnostic endoscopies.
North America continues to lead in terms of unit cost, with average colonoscope prices between $20,000 and $28,000. This trend is sustained by demand for advanced features such as 4K visualization, narrow-band imaging, and AI-based lesion detection. The Centers for Disease Control and Prevention (CDC) in the U.S. recommends routine colorectal cancer screening starting at age 45, expanding the eligible patient population. Increased screening volumes have driven procurement cycles, stabilizing demand even in economic downturns.
In Europe, prices range from $18,000 to $25,000. The European Union’s focus on medical device regulation (MDR) and strict CE certification standards adds compliance costs for manufacturers. However, national health systems frequently negotiate bulk contracts, stabilizing long-term pricing. Germany, France, and the U.K. represent the largest European markets, each prioritizing advanced visualization systems for tertiary care centers.
Asia presents more dynamic price trends. In Japan, colonoscope technology is at the forefront, with domestic manufacturers such as Olympus and Fujifilm producing premium systems priced at $22,000–$30,000. China, meanwhile, has expanded local manufacturing capabilities, offering competitive models priced at $12,000–$18,000, significantly undercutting international brands. India and Southeast Asia remain cost-sensitive markets, with refurbished and mid-tier models dominating purchases.
Disposable colonoscopes, priced per unit at approximately $250–$400, are increasingly trialed in the U.S. and Western Europe. While their adoption remains limited, infection control protocols and the COVID-19 pandemic experience have heightened interest. Hospitals adopting disposable scopes reduce sterilization infrastructure costs but face higher per-procedure expenses.
Colonoscope pricing is best understood through structured analysis across product tiers.
Priced between $8,000 and $12,000, these scopes are equipped with HD imaging, standard angulation controls, and compatibility with basic processors. They are designed for small clinics and facilities with limited patient volumes. Their affordability makes them attractive to resource-limited settings, but their functionality is often insufficient for advanced diagnostic and therapeutic interventions.
Ranging from $15,000 to $22,000, mid-tier scopes offer improved maneuverability, compatibility with 4K-capable processors, and enhanced durability. They are widely adopted in regional hospitals and community healthcare centers. These models balance cost and performance, offering extended lifespans and lower maintenance needs compared to entry-level equipment.
Premium colonoscopes exceed $25,000, reaching up to $35,000. They feature 4K resolution, AI-enhanced visualization, advanced imaging modes such as narrow-band imaging, and high durability designed for high-volume tertiary hospitals. Their integration with hospital electronic health record (EHR) systems and cloud-based platforms further justifies their pricing.
Refurbished colonoscopes, priced between $5,000 and $10,000, remain popular in cost-sensitive regions. They provide reliable performance for basic screening but may lack warranty coverage or the latest imaging technologies. Hospitals considering refurbished options must weigh lower upfront costs against potentially higher maintenance risks.
With costs ranging from $250–$400 per procedure, disposable colonoscopes introduce a variable pricing model. Their adoption reduces sterilization and cross-contamination risks but increases per-patient expenditure. While not yet mainstream, they are gaining traction in infectious disease-sensitive contexts.
| Category | Price Range (USD) | Features | Suitable Facilities |
|---|---|---|---|
| Entry-Level HD | $8,000–$12,000 | Basic HD imaging, standard features | Small clinics |
| Mid-Tier | $15,000–$22,000 | 4K-ready, ergonomic, durable | Regional hospitals |
| High-End 4K + AI | $25,000–$35,000 | AI imaging, NBI, cloud integration | Tertiary hospitals |
| Refurbished | $5,000–$10,000 | Reliable but older models | Cost-sensitive facilities |
| Disposable Units | $250–$400 each | Infection control, single-use | Specialized centers |
 Colonoscope Price Factors
Colonoscope Price FactorsResolution is the single most important factor affecting cost. HD colonoscopes remain sufficient for routine screening, but 4K visualization systems provide enhanced detection of flat lesions and small polyps. Narrow-band imaging, chromoendoscopy, and AI-assisted recognition further increase device cost. Durability, reprocessing efficiency, and compatibility with high-level disinfectants also contribute to higher prices.
In 2025, the colonoscope market shows a clear distinction between international suppliers and regional factories. While many global companies remain active, hospitals and distributors are increasingly turning to competitive Asian production. Among them, XBX has built a strong reputation as a reliable colonoscope supplier, colonoscope manufacturer, and colonoscope factory, offering solutions that combine quality assurance with cost efficiency.
Choosing the right supplier or manufacturer is a key colonoscope price factor. Working directly with a colonoscope factory such as XBX reduces intermediary costs, improves delivery times, and ensures better customization through OEM and ODM models. Hospitals and clinics that cooperate with established colonoscope suppliers gain access to stronger service networks, extended warranties, and compliance support for FDA, CE, and ISO standards.
For procurement managers, comparing colonoscope price strategies across suppliers and evaluating the total cost of ownership are essential steps. XBX, as a trusted colonoscope manufacturer, supports buyers with transparent quotations, factory-direct pricing, and comprehensive after-sales service. This approach helps healthcare providers achieve both affordability and clinical quality in 2025.
Procurement teams must account for full system costs. A colonoscope requires a compatible processor ($8,000–$12,000), light source ($5,000–$10,000), and monitor ($2,000–$5,000). Maintenance contracts can add $3,000–$5,000 annually. Staff training programs, sterilization systems, and consumables contribute additional expenditures. Over a 5-year lifecycle, total ownership costs may exceed double the initial purchase price.
FDA, CE, and ISO certifications influence price. Compliance requires clinical trials, quality testing, and documentation, all of which are reflected in retail pricing. Non-certified or locally approved devices may cost less but carry reputational and liability risks.
Large hospitals benefit from bulk procurement, negotiating 10–15% discounts on multi-unit contracts. Health networks often pool resources to secure larger contracts. Smaller clinics, while unable to negotiate volume discounts, may benefit from long-term partnerships with local distributors.
Leasing agreements and financing arrangements allow hospitals to spread costs over 3–5 years. Refurbished units offer entry points for resource-limited institutions. Service-inclusive contracts, though raising initial costs, stabilize long-term budgets. Some hospitals also adopt mixed fleets of new, refurbished, and disposable scopes, balancing performance with budget control.
Direct purchasing from manufacturers or OEM factories bypasses distributor markups, reducing costs by up to 20%. Negotiation strategies increasingly include non-price elements such as extended warranties, free training, and guaranteed spare part delivery timelines. In competitive markets, suppliers are more willing to customize agreements, giving hospitals leverage.
Hospitals also evaluate risk in procurement strategies. Single-supplier dependency can create vulnerability in case of supply disruptions. Diversifying suppliers across regions and including both premium and mid-tier manufacturers provides stability.
Average colonoscope costs range between $20,000 and $28,000. Hospitals prioritize advanced systems with 4K, AI features, and integrated cloud data storage. Regulatory approval requirements and higher labor costs contribute to elevated pricing.
Prices remain in the $18,000–$25,000 range. EU regulatory frameworks ensure high compliance costs. National health services negotiate long-term agreements, often securing favorable terms for bulk purchases.
Japan’s premium models are priced at $22,000–$30,000. China offers mid-tier systems at $12,000–$18,000, with competitive quality. India and Southeast Asia rely heavily on refurbished and entry-level models due to budget constraints.
In Africa and Latin America, colonoscope prices are highly variable. Donor-funded programs and NGO support often provide refurbished or discounted equipment. Disposable scopes are rarely adopted due to per-procedure costs.
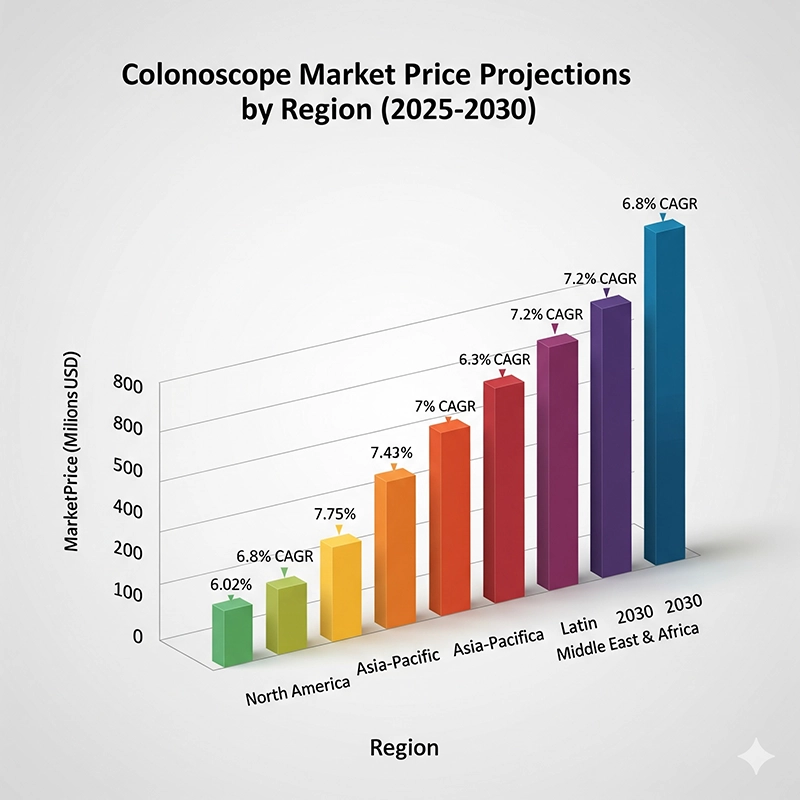
From 2025 to 2030, the colonoscope market is projected to expand at a compound annual growth rate (CAGR) of 5–7%. According to IEEE HealthTech, AI-assisted visualization could become standard in tertiary hospitals within five years, raising baseline costs. Statista projects Asia-Pacific to account for the fastest market growth due to expanding healthcare infrastructure.
Emerging innovations such as wireless colonoscopes, cloud-based reporting, and robotic-assisted navigation are in development. These technologies may further increase procurement costs but improve diagnostic accuracy and patient safety. Disposable colonoscopes may see wider adoption if unit costs decline through mass production, potentially reshaping infection control strategies.
| Region | 2025 Avg Price (USD) | 2030 Projected Avg Price (USD) | CAGR (%) | Key Drivers |
|---|---|---|---|---|
| North America | $24,000 | $29,000 | 4.0 | AI adoption, FDA compliance |
| Europe | $22,000 | $27,000 | 4.2 | MDR compliance, bulk contracts |
| Asia-Pacific | $16,000 | $22,000 | 6.5 | Expanded screening, local manufacturing |
| Latin America | $14,000 | $18,000 | 5.0 | NGO programs, refurbished adoption |
| Africa | $12,000 | $16,000 | 5.5 | Donor support, cost-sensitive procurement |
Understanding the colonoscope price in 2025 is about more than the sticker on a device. A colonoscopy is a workflow that blends clinical labor, sterile processing, diagnostics, and capital equipment. A basic portable HD colonoscope can cost around USD 2,900, mid-tier systems run USD 15,000–22,000, and high-end integrated 4K/AI platforms reach USD 25,000–35,000. Yet patients rarely see “device price” on their bill. Instead, they encounter the accumulated costs of facilities, clinicians, anesthesia, pathology, and prep/follow-up visits—magnified or moderated by insurance policy design.
Below is a practical, numbers-first view of how those costs stack up, and how hospitals can plan purchases, budgets, and ROI.
While costs vary by region and hospital type, U.S. national averages provide a useful baseline. Synthesizing fee schedules and typical facility charges, the breakdown often looks like this:
| Cost Component | Estimated Share of Total (%) | Typical Range (USD) | What It Covers |
|---|---|---|---|
| Facility fees | 35–45% | 700–2,000 | Endoscopy suite time, recovery bay, capital amortization, nursing/tech staffing, cleaning/turnover |
| Physician + anesthesia | 20–25% | 400–1,200 | Gastroenterologist professional fee; anesthesia professional + drugs (propofol/monitored anesthesia care) |
| Pathology/biopsy | 10–15% | 200–700 | Lab processing and histology if tissue is removed; multiple samples increase cost |
| Pre-/post-consults | 5–10% | 100–300 | Initial evaluation, prep instructions, post-procedure visit |
| Patient out-of-pocket | 5–15% | 150–800 | Deductible/coinsurance for diagnostic coding or out-of-network services |
| Geography effect | — | ±20–30% | Urban academic centers trend higher; rural ambulatory centers trend lower |
Illustrative average (U.S., 2025): a total bill of USD 2,500–5,000 might break down as ~USD 1,200 facility (40%), ~USD 800 professional/anesthesia (25%), ~USD 400 pathology (15%), ~USD 200 consults (7%), and ~USD 400 patient liability (13%). In practice, the single largest driver is where the procedure occurs—hospital outpatient department vs ambulatory surgery center—because labor rates, overhead, and capital allocations differ.
What changes the percentages?
Therapeutic colonoscopies (extensive polypectomy, clip placement) push professional and pathology shares up.
High-volume centers tame facility shares via throughput and faster room turnover.
Deep sedation increases anesthesia costs; moderate sedation performed by the endoscopy team trims that share.
Value-based contracts (bundled payments) compress variation by fixing the total allowed amount.
The colonoscope price reflects more than optics:
Entry HD (~USD 2,900–12,000): Sufficient for routine screening; modest durability; basic processors/light sources.
Mid-tier (USD 15,000–22,000): Better ergonomics, wider angulation, tougher insertion tube materials, compatibility with 4K processors.
High-end 4K + AI (USD 25,000–35,000): Advanced imaging modes (e.g., NBI/digital chromoendoscopy), AI-assisted polyp detection, integration with EHR/PACS, hardened design for high-cycle reprocessing.
Refurbished (USD 5,000–10,000): Attractive for budget-limited centers; key is verified service history, leak-test integrity, and a real warranty.
Disposable scopes (USD 250–400 per case): Remove reprocessing risk; viable where infection-control premiums or labor constraints are high.
| Category | Average Price (USD) | Typical Use Cases |
|---|---|---|
| Entry-Level HD | 2,900 – 12,000 | Small clinics, routine screenings |
| Mid-Tier | 15,000 – 22,000 | Regional hospitals, balanced performance |
| High-End 4K + AI | 25,000 – 35,000 | Tertiary hospitals, advanced diagnostics |
| Refurbished | 5,000 – 10,000 | Cost-sensitive facilities |
| Disposable Units | 250 – 400 per procedure | Specialized infection-control use |
Don’t forget the stack: processors USD 8,000–12,000, light sources USD 5,000–10,000, medical-grade displays USD 2,000–5,000. Many buyers underestimate how much of the final image quality depends on the processor pipeline and display—not just the insertion tube.
Because the device is used thousands of times, the purchase price becomes only one part of economics. A simple but realistic five-year TCO model helps compare options:
| TCO Element (5 years) | Entry HD System | Mid-Tier System | 4K + AI System |
|---|---|---|---|
| Device purchase (scope + stack) | 12,000–18,000 | 20,000–30,000 | 30,000–45,000 |
| Annual service contracts | 8,000–12,500 | 12,500–20,000 | 15,000–25,000 |
| Repairs/consumables | 3,000–6,000 | 4,000–8,000 | 6,000–10,000 |
| Staff training/competency | 3,000–6,000 | 4,000–8,000 | 6,000–10,000 |
| Sterile processing/upgrades | 4,000–8,000 | 5,000–10,000 | 7,000–12,000 |
| Five-year TCO (range) | 30,000–50,000 | 45,000–76,000 | 64,000–102,000 |
Two practical observations:
Service levels (response time, loaner scope availability) are worth paying for in high-volume centers where downtime is extremely expensive.
Training isn’t optional—AI and advanced imaging modes pay off only when endoscopists and nurses routinely use them.
United States. Preventive screening colonoscopies are generally covered without cost-sharing under the ACA. However, the moment a polyp is removed, some plans recode the claim as diagnostic, which can trigger coinsurance. Out-of-pocket for insured patients often lands in the USD 1,300–1,500 band; uninsured patients may see USD 4,000+ bills. Medicare covers the exam but may not recognize price differences between HD vs 4K/AI systems—the hospital absorbs tech premiums inside the facility fee.
Europe. Public payers cover the bulk of costs. Out-of-pocket is typically a nominal co-pay. Procurement is centralized; pricing is stabilized via tenders and multi-year contracts. The patient experience is largely shielded from equipment list prices.
Asia-Pacific. Japan’s national insurance supports high screening rates, and hospitals invest in top-tier imaging to maintain quality. In China, tier-3 urban hospitals adopt 4K/AI systems rapidly, while county hospitals often deploy mid-tier or refurbished scopes; patient self-pay remains significant outside major metros. In India and parts of Southeast Asia, insurance penetration is lower, so affordability pressures tilt providers toward mid-tier/refurbished equipment.
Latin America & Africa. Mixed public/private financing produces wide variability. Donor programs and NGOs frequently seed capacity with refurbished systems; when volumes grow, hospitals migrate to mid-tier stacks and stronger service coverage.
Bottom line: insurance design—not the colonoscope price alone—determines a patient’s bill. For hospitals, reimbursement rates, not list prices, decide ROI.
Four levers move ROI more than any single price tag:
Throughput. Faster room turnover and standardized sedation/protocols can increase daily cases 15–30%, diluting fixed facility costs.
Detection yield. 4K/AI systems modestly improve adenoma detection rates (ADR) in many settings; fewer missed lesions can reduce follow-up procedures and downstream costs.
Uptime. Service contracts with 24–48-hour loaner guarantees protect revenue. A busy unit losing three days of scopes can forfeit five figures of reimbursement.
Case mix. Therapeutic colonoscopies reimburse more; centers with advanced tools (EMR kits, clipping devices) offset capital costs faster.
Three scenario sketches (5-year horizon):
High-volume tertiary center (3 rooms × 12 cases/day, 250 days/year = 9,000 cases/year): even a USD 90k TCO for a 4K+AI system pays for itself quickly because downtime is costly and marginal detection gains matter for outcomes and quality metrics.
Regional hospital (1 room × 8 cases/day, 200 days/year = 1,600 cases/year): USD 60k TCO mid-tier system yields robust ROI if service coverage is right-sized and staff use advanced modes consistently.
Community ASC (1 room × 5 cases/day, 180 days/year = 900 cases/year): a USD 35–45k TCO entry/mid hybrid with a strong refurb program can be optimal, especially with cash-pay patients.
A quick back-of-the-envelope. If average net margin per case is USD 250–400 after variable costs, then 1,600 cases/year produce USD 400k–640k contribution. The capital decision becomes about protecting that flow with uptime, workflow, and adequate imaging—not chasing specs that won’t be used.
Reusable scopes require high-level disinfection, leak testing, and meticulous handling. Each cycle has a labor + consumable cost (often USD 25–45 per turn) plus periodic repairs. The hidden number is damage rate—a few mishandled scopes can erase the savings from buying cheaper equipment.
Disposable scopes remove reprocessing risk and can free staff time; they shine in ambulatory centers with limited sterile processing or in outbreaks where infection control carries a premium. But at USD 250–400 per case, the breakeven vs reusable scopes typically requires either a very high labor/repair environment or specific infection-control policies that monetize risk reduction.
Hybrid fleets (reusable as the backbone, disposable for selected cases, e.g., isolation rooms) are an increasingly common compromise.
Bulk buys and framework agreements. Health systems pooling demand routinely secure 10–15% unit discounts and better service terms. Use multi-year volume commitments to unlock loaner pools and faster on-site response.
Leasing/managed service. Three- to five-year leases bundle service and allow mid-term upgrades. Cash-flow-friendly for clinics expanding capacity without capex spikes.
OEM/ODM partnerships. Factory-direct supply can cut intermediaries and tailor builds (connectors, software, training content). Brands like XBX frequently offer customization and responsive support in exchange for clearer forecasts and training commitments.
Required imaging modes (HD/4K, NBI/digital chromo) and AI module availability
Compatibility with existing processors and washers
Service SLAs (response time, loaners, preventive maintenance cadence)
Training scope (initial + refreshers, on-site vs remote)
Warranty terms (insertion tube coverage, parts availability horizon)
Data integration (EHR/PACS export, cybersecurity posture)
Negotiation levers. Package pricing (scope + processor + light source), extended warranty years, spare insertion tubes, and on-site trainer days tend to be higher-value than a small headline discount.
North America: Device list prices and facility charges are highest. Buyers emphasize SLAs and downtime protection; AI add-ons are common in academic centers.
Europe: Centralized tenders compress prices and standardize configurations. MDR compliance adds supplier cost but reduces variability for hospitals.
Asia-Pacific: Rapid growth with a two-track pattern—Japan at the premium end; China and Korea offering competitively priced mid- to high-tier systems; India/Southeast Asia balancing refurbished with selective new acquisitions.
Latin America/Africa: Refurbished fleets dominate early expansion; as programs mature, hospitals layer in mid-tier stacks with better service coverage.
This diversity matters because a colonoscope price quoted in one market can translate into very different hospital economics elsewhere.
Pricing trajectory. Expect stable entry-level device pricing (tight manufacturing and global competition) and gradual increases in high-end platforms as AI modules, better sensors, and data-security features accrue. Hospitals will scrutinize whether AI improves ADR in their hands—if yes, the capital premium is easier to justify.
Workflow dominance. The winners won’t just have sharper images; they’ll ship with training pathways, analytics on withdrawal time/ADR, and easier data export. In other words, price follows workflow value.
Service as strategy. With staff shortages, service offerings that include on-site trainers, rapid loaners, and proactive maintenance will be valued at a premium. Contracts that guarantee uptime are effectively insurance for revenue.
Disposable threshold. If unit cost drops close to USD 200 and hospitals can repurpose SPD labor, a broader shift toward single-use could emerge in targeted settings (isolation rooms, satellites, high turnover lists).
What to do now. Tie any purchase to measurable outcomes: ADR improvement goals, room-turnover KPIs, uptime SLAs, and staff competency metrics. That’s how leadership justifies spend even when budgets are tight.
For patients:
Ask your insurer if your exam will be coded as preventive or diagnostic—that single detail often determines whether you pay USD 0 or several hundred dollars.
Hospital outpatient departments cost more than ambulatory centers; if medically appropriate, shop facility type.
For hospitals/clinics:
Model five-year TCO; don’t buy features you won’t use.
Protect throughput with service SLAs and training.
Consider OEM/ODM for tailored value; standardize across rooms to simplify SPD and training.
Track ADR and room turnover; make technology earn its keep.
Bottom line: The colonoscope price is one lever inside a larger system of clinical quality, workflow, staffing, and reimbursement. Plan purchases against TCO and measurable outcomes, and the economics—both patient-facing and hospital-level—fall into place.
Colonoscope pricing in 2025 reflects a balance of technology, manufacturing, regional economics, and procurement strategies. Hospitals face a wide spectrum of options, from refurbished entry-level devices to premium AI-enabled systems. Procurement teams must evaluate total ownership costs, including service, training, and consumables, rather than relying solely on sticker price.
Price trends indicate gradual upward movement, particularly for high-end devices, driven by AI and 4K integration. However, competition from Asian manufacturers and refurbished markets continues to provide affordable entry points. Strategic purchasing approaches—bulk procurement, leasing, and direct sourcing—offer significant opportunities to control expenditure.
Ultimately, colonoscope procurement in 2025 requires nuanced analysis. By combining awareness of global price trends, careful evaluation of influencing factors, and implementation of cost-effective strategies, hospitals and clinics can ensure that their investments deliver both financial efficiency and clinical excellence.
Colonoscopes generally range from $8,000 to $35,000 depending on resolution (HD vs 4K), imaging modes, durability, and manufacturer. Refurbished models are available at $5,000–$10,000, while disposable scopes cost $250–$400 per procedure.
A colonoscope requires processors ($8k–12k), light sources ($5k–10k), and monitors ($2k–5k). Annual service contracts ($3k–5k), sterilization equipment, and training fees are also common. Total cost of ownership can be 2x the purchase price over 5 years.
Disposable scopes cost $250–$400 per unit and eliminate reprocessing needs, ideal for infection-sensitive settings. Reusable scopes have higher upfront costs but lower per-procedure expenses in high-volume hospitals.
Colonoscope price factors include processors ($8k–12k), light sources ($5k–10k), monitors ($2k–5k), annual service ($3k–5k), sterilization equipment, and training. Over a 5-year lifecycle, the total cost of ownership may double the initial colonoscope price.
Colonoscope price trends 2025 show that North America averages $20k–28k, Europe $18k–25k, Japan $22k–30k, China $12k–18k. Regional colonoscope price factors include import taxes, certifications, and supplier strategies.
Most colonoscope suppliers include on-site installation and staff training in the colonoscope price strategies. OEM/ODM colonoscope manufacturers may also provide digital training or extended service contracts.
Copyright © 2025.Geekvalue All rights reserved.Technical Support:TiaoQingCMS