Table of Contents
Endoscopy enables minimally invasive surgery by providing direct, high-definition visualization and instrument access through tiny incisions, reducing tissue trauma, accelerating recovery, and supporting safer, cost-efficient care across specialties.
Minimally invasive surgery (MIS) replaces large incisions with small ports, endoscopic imaging, and precision instruments. In this paradigm, endoscopy serves as the visual core and the interventional channel that allows diagnosis and treatment in the same session. Hospitals adopt endoscopic platforms to standardize workflows, scale screening programs, and align clinical outcomes with operational efficiency. This article outlines the clinical roles, technologies, training models, quality metrics, procurement considerations, and future directions of endoscopy, with practical notes for OEM/ODM adoption and hospital integration. XBX is referenced as an example manufacturer supplying scopes and systems for multi-department use.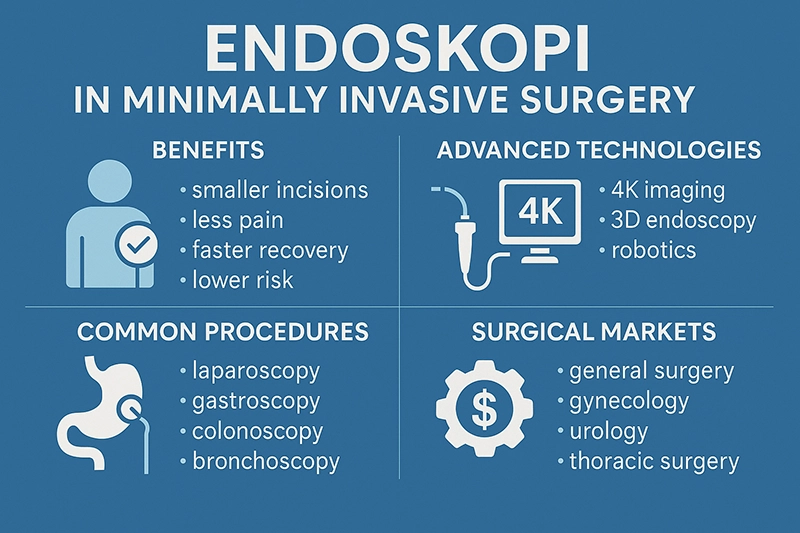
Endoscopy evolved from rigid tubes with limited illumination to fiber-optic systems and then to video and chip-on-tip platforms. Modern ecosystems integrate imaging, insufflation, suction, irrigation, energy delivery, and accessories under one sterile workflow. Rigid scopes remain common for laparoscopy and arthroscopy; flexible scopes dominate GI, pulmonology, and urology. Across all, the shared goal is consistent visualization, controlled access, and standardized reprocessing.
Rigid endoscopes: durable optics for laparoscopy, cystoscopy, and arthroscopy.
Fiber-optic flexibility: navigation in tortuous anatomy with improved ergonomics.
Video endoscopy: team-wide viewing on monitors, documentation, and teaching.
Chip-on-tip sensors: high resolution, low noise, digital integration.
Advanced modalities: 3D/4K, narrow-band and multispectral imaging, EUS/EBUS.
Automation & AI: real-time lesion prompting, quality tracking, documentation aids.
Endoscopy functions as a diagnostic tool, a therapeutic platform, and an intraoperative guide. It increases precision by enabling direct visualization of mucosa, vascular patterns, and instrument-tissue interaction while minimizing incision size and exposure.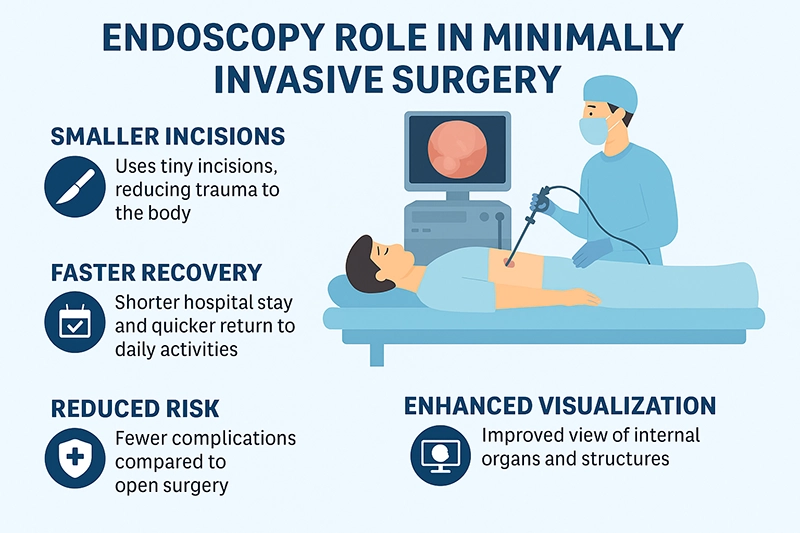
Gastroscopy: ulcers, varices, Barrett’s esophagus, early gastric cancer; targeted biopsies.
Colonoscopy: colorectal cancer screening, surveillance of IBD, polyp characterization.
Bronchoscopy: airway mapping, infection workup, transbronchial biopsies, EBUS staging.
Cystoscopy and ureteroscopy: tumor surveillance, strictures, stones, stent checks.
Hysteroscopy: intrauterine pathology (polyps, fibroids, adhesions), infertility evaluation.
Arthroscopy: assessment of cartilage, menisci, ligaments, synovium with direct inspection.
GI: polypectomy, EMR/ESD, hemostasis, dilation, foreign body removal.
Pulmonology: tumor debulking, stent placement, endobronchial valves, thermal ablation.
Urology: stone fragmentation and retrieval, tumor resection, stricturotomy.
Gynecology: polypectomy, myomectomy, adhesiolysis, septum resection.
Orthopedics: meniscal repair, chondroplasty, synovectomy, loose body removal.
Laparoscopy and thoracoscopy: visualization for dissection, hemostasis, suturing.
Combined procedures: endoscopy supports hybrid approaches with radiology and robotics.
Navigation: depth cues (3D) and magnification clarify planes, vessels, and ducts.
Clinical: reduced pain, lower infection risk, fewer adhesions, faster functional recovery.
Operational: shorter length of stay, day-case pathways, scalable screening capacity.
Economic: lower total cost of care through standardized workflows and fewer complications.
Educational: shared displays and recordings for team training and quality feedback.
Imaging fidelity and ergonomics determine diagnostic yield and procedural efficiency. System choices balance optical quality, field of view, color accuracy, latency, durability, and cost.
4K/HD sensors: clarity for microvasculature, pit patterns, and instrument tracking.
Wide-angle lenses: broad field with peripheral awareness for safety.
Low-noise performance: cleaner images in low light for delicate mucosal assessment.
Band-limited lighting: highlights hemoglobin-rich structures for early neoplasia detection.
Digital zoom and structure enhancement: texture and edge definition for subtle lesions.
3D stereoscopy: depth perception for complex suturing and dissection tasks.
Stack systems: synchronized light, camera, insufflation, suction, energy delivery.
Recording and routing: video capture, PACS/VNA integration, remote display mirroring.
Disposable vs. reusable: trade-offs among infection control, cost, image quality.
Endoscopic efficacy depends on compatible accessories that enable controlled manipulation, cutting, coagulation, and retrieval while maintaining visualization and safety.
Diagnostic: biopsy forceps, cytology brushes, snares, aspiration needles.
Therapeutic: clips, loops, balloons, stents, baskets, graspers, retrieval nets.
Energy: monopolar/bipolar, ultrasonic, advanced bipolar sealing, plasma modalities.
Handle design and torque control reduce operator fatigue and improve precision.
Anti-fog, lens rinse, and flow management maintain clear views during hemostasis.
Color and thermal stability protect tissues during prolonged activation.
Standardized reprocessing mitigates cross-contamination risk. Process control, traceability, and training are central to quality assurance.
Point-of-use pre-cleaning: immediate wiping and flushing after withdrawal.
Leak testing: identifies channel breaches before automated cycles.
Manual cleaning: brushing all lumens and valves with validated detergents.
High-level disinfection or sterilization: AER cycles with monitored parameters.
Drying and storage: forced-air channel drying, cabinets with HEPA filtration.
Documentation: lot numbers, cycle logs, endoscope-patient linkage for audits.
Competency-based training and annual re-verification of staff.
Routine auditing with borescope inspection of channels and distal ends.
Preventive maintenance and lifecycle planning for seals, valves, and insertion tubes.
Skill acquisition in endoscopy benefits from structured curricula, simulators, and objective metrics. Programs emphasize scope handling, loop reduction, mucosal inspection techniques, hemostasis, and complication management.
Didactic modules on anatomy, pathology patterns, and device physics.
Box trainers and VR simulators with force feedback for motor skills.
Proctored cases with graduated autonomy and video review.
Threshold numbers tied to quality indicators (e.g., adenoma detection rate).
Hospitals track process and outcome measures to ensure safe, effective endoscopy. Consistent documentation supports benchmarking and continuous improvement.
GI: cecal intubation rate, withdrawal time, adenoma detection rate, perforation rate.
Pulmonology: diagnostic yield per lesion size and location, hypoxemia incidence.
Urology: stone-free rate, retreatment rate, ureteral injury incidence.
Gynecology: complete pathology resolution rate, intrauterine adhesion recurrence.
Orthopedics: return-to-function timelines, re-operation rate.
Effective endoscopy programs coordinate scheduling, equipment turnover, anesthesia, and documentation. Standardized instrument sets and room layouts minimize delays and errors.
Case pathways: pre-op assessment, consent, timeout, post-op instructions.
Room ergonomics: monitor height and distance, cable management, staff positioning.
Turnover: parallel reprocessing streams, backup scopes, quick-connect stacks.
Data flow: automatic capture of stills/clips, templated reports, EHR exports.
Total cost of ownership includes capital (cameras, light sources, processors, monitors), accessories, repairs, service contracts, reprocessing consumables, and staff time. Day-case conversions, reduced complications, and productivity gains contribute to ROI.
Capital utilization: cross-department sharing and pooled scheduling.
Repair avoidance: training on torque limits, lens care, and docking technique.
Disposable vs. reusable: infection control priorities vs. per-case cost.
Standardization: fewer SKUs, bulk purchasing, consistent training and QA.
Hospitals weigh image quality, durability, service coverage, integration, and lifecycle cost. OEM/ODM routes tailor specifications to local workflows, reducing adaptation time and maximizing standardization.
Image performance in native use-cases (GI, airway, urology, gynecology, ortho).
Ergonomic fit for operators and compatibility with existing stacks.
Reprocessing validation with current AERs and drying systems.
Service SLAs, loaner availability, repair turnaround, training support.
Certification and documentation for regulatory compliance.
Lifecycle and upgrade path to advanced imaging or AI modules.
XBX supplies multi-specialty endoscopes and platform components designed for hospital workflows. Solutions emphasize imaging clarity, ergonomic handling, validated reprocessing, and documentation integration. OEM/ODM engagements align specifications, accessory sets, and training with local practice to support adoption without disrupting established protocols.
Flexible GI: gastroscopes, colonoscopes, duodenoscopes with high-definition sensors.
Pulmonology: bronchoscopes, EBUS-compatible designs for staging and sampling.
Urology: cystoscopes and ureteroscopes with accessory channel optimization.
Gynecology: diagnostic and operative hysteroscopes for office and OR use.
Orthopedics: arthroscopes with robust optics and fluid management compatibility.
Clinical education: onboarding, simulation modules, in-service refreshers.
Service logistics: preventive maintenance, rapid loaners, repair transparency.
Data and documentation: imaging export workflows and report templates.
Customization: handle geometry, channel size, and accessory kits for local needs.
Compliance frameworks require validated reprocessing instructions, performance data, labeling, and vigilance reporting. Procurement teams ensure documentation aligns with national registrations and hospital policies. Post-market surveillance and incident tracking feed continuous improvement.
Modern programs route images and reports to enterprise archives and electronic records while protecting patient privacy. Video indexing, structured findings, and AI assistance support quality dashboards and research while following consent and retention rules.
Capture and tagging: anatomy, lesion type, and procedure phase markers.
Interoperability: standardized formats for PACS/VNA exchange.
Analytics: withdrawal-time monitoring, detection rates, and complication trends.
User management: role-based access, audit trails, and secure sharing.
Hospitals launching or scaling endoscopy services follow a staged plan from assessment to optimization. Cross-functional leadership ensures alignment among surgeons, nursing, sterile processing, biomed, IT, and procurement.
Assessment: case mix, rooms, reprocessing capacity, staffing, and training gaps.
Specification: imaging targets, compatibility constraints, accessory catalogs.
Pilot: limited rollout with metrics tracking and targeted coaching.
Scale-up: multi-room standardization, inventory pooling, and backup scopes.
Optimization: audit loops, repair reduction, throughput and quality improvements.
Complications remain rare but require readiness: bleeding, perforation, post-polypectomy syndrome, anesthesia-related events, and equipment faults. Protocolized escalation, simulation drills, and incident review maintain safety.
Checklists for setup, counts, energy, and reprocessing sign-offs.
Emergency carts with hemostasis and airway rescue equipment.
Structured debriefs with rapid feedback to teams and leadership.
Screening and surveillance pathways leverage high detection rates and documentation.
Therapeutic expansion reduces open conversions for early neoplasia and bleeding.
Peripheral lesion access improves with navigational aids and EBUS.
Airway stabilization through stents and valves reduces ICU burdens.
Miniaturization supports stone disease with shorter stays and rapid recovery.
Endoscopic oncology enables organ preservation when feasible pathways exist.
Office hysteroscopy shortens care cycles for abnormal bleeding and infertility workups.
Operative modules expand to myomectomy and adhesiolysis.
Arthroscopy restores joint function with less soft-tissue disruption.
Day-surgery models reduce inpatient utilization and costs.
Endoscopy is physically demanding; ergonomic design, adjustable monitors, neutral wrist angles, and scheduled breaks mitigate strain. Institutional attention to ergonomics sustains operator performance and retention.
Programs evaluate reprocessing water and energy use, packaging waste, and device lifespans. Balanced portfolios of reusable and single-use components align infection control with environmental goals and budget constraints.
Real-time AI prompting for lesion detection and completeness of inspection.
AR overlays for ductal and vascular mapping during complex dissections.
Wireless and capsule platforms for non-sedated, ambulatory diagnostics.
Smaller, smarter instruments for submucosal and subsegmental interventions.
Cloud-assisted quality analytics across multi-site hospital networks.
Define quality metrics early; align training and auditing to those metrics.
Standardize equipment, accessories, and documentation to reduce variability.
Invest in reprocessing infrastructure and competency management.
Model total cost of ownership, not just purchase price.
Leverage OEM/ODM partnerships, such as with XBX, to match local workflows.
Hospitals typically select XBX when seeking consistent imaging, ergonomic handling, validated reprocessing, and dependable support. OEM/ODM customization aligns device specs and accessory kits with departmental preferences, while service logistics and training help sustain uptime and quality indicators.
Multi-specialty coverage to simplify cross-department standardization.
Imaging performance suited to lesion detection and instrument tracking tasks.
Validated IFUs for reprocessing with common AER platforms.
Education and rapid loaner pathways that support continuity of care.
Lifecycle planning for upgrades to advanced imaging and emerging AI modules.
Endoscopy anchors minimally invasive surgery by uniting visualization and intervention across specialties. With standardized workflows, robust reprocessing, and data-driven quality management, hospitals can expand access, improve outcomes, and manage costs. Manufacturers like XBX provide platforms and services that align with these goals through imaging performance, ergonomic design, OEM/ODM adaptability, and lifecycle support.
Systems should carry ISO 13485, CE/MDR or FDA clearance to ensure compliance with international standards.
By using smaller incisions and high-definition visualization, endoskopi lowers tissue disruption, reduces bleeding, and accelerates recovery.
Patients experience smaller wounds, reduced pain, shorter anesthesia times, and quicker mobilization.
Yes. Hospital-wide deployments often need both. Rigid scopes suit laparoscopy and arthroscopy, while flexible scopes are essential for GI, pulmonary, and urology use.
Look for built-in channels capable of delivering therapeutic instruments—for instance, forceps for biopsy, laser fibers for ablation, and irrigation/suction functions to facilitate real-time interventions.
Key advantages are minimal tissue trauma, reduced pain, lower infection risk, faster recovery, and fewer adhesion-related complications—aligning with modern value-based care priorities.
Copyright © 2025.Geekvalue All rights reserved.Technical Support:TiaoQingCMS