Table of Contents
Bariatric endoscopy is a minimally invasive medical procedure that enables physicians to perform weight loss interventions inside the stomach without external incisions. It is considered an alternative to bariatric surgery, designed for patients who struggle with obesity and require effective treatment beyond diet and exercise. Hospitals and clinics increasingly adopt bariatric endoscopy as part of their obesity management programs, offering patients faster recovery times, fewer risks, and access to advanced medical technology.
Bariatric endoscopy refers to a set of therapeutic procedures carried out with a flexible endoscope, a medical device inserted through the mouth and advanced into the stomach. The primary goal is to reduce the effective capacity of the stomach or to modify its function, helping patients achieve weight loss in a safe and controlled manner.
Unlike bariatric surgery, which involves invasive techniques such as cutting or stapling sections of the stomach, bariatric endoscopy relies on minimally invasive methods. With the support of advanced imaging and specialized instruments integrated into systems like the XBX endoscope, physicians can suture, reshape, or insert devices into the stomach while maintaining a natural anatomy.
Minimally invasive approach:procedures are performed without abdominal incisions。
Endoscopic visualization:real-time imaging ensures precise control and safety。
Temporary or reversible interventions:some methods, like intragastric balloons, can be removed once treatment goals are met。
Reduced patient burden:shorter recovery times and fewer complications compared with surgery。
These principles position bariatric endoscopy as a practical solution for patients who are not candidates for surgery but still require effective obesity management.
Bariatric endoscopy is increasingly recommended because it bridges the gap between lifestyle modification and invasive surgery. For many patients, diet and exercise alone do not deliver sufficient weight loss, while surgery may be too risky or undesirable. Bariatric endoscopy offers a middle ground.
Clinical necessity:addresses obesity-related complications such as diabetes, hypertension, and sleep apnea。
Stomach volume reduction:procedures like endoscopic sleeve gastroplasty reduce the stomach’s capacity, helping patients feel full sooner。
Safety:no external cuts or stitches, resulting in fewer risks of infection and minimal bleeding。
Faster recovery:many patients can return to work and normal activities within a few days。
Revisional option:can correct or adjust prior bariatric surgeries when initial results are unsatisfactory。
Healthcare efficiency:outpatient treatment models reduce bed occupancy and overall costs。
By combining clinical safety with patient convenience, bariatric endoscopy has become an essential tool in modern obesity treatment, supporting both individuals and healthcare providers in managing the global obesity challenge.
Bariatric endoscopy combines advanced imaging, precision instruments, and minimally invasive techniques to achieve meaningful weight loss. A flexible endoscope equipped with a high-definition camera and specialized tools is introduced through the patient’s mouth and guided into the stomach. This allows real-time visualization of the gastrointestinal tract and targeted interventions without external incisions.
Physicians use suturing devices attached to the endoscope to fold and stitch the stomach walls, creating a smaller, tube-like shape.
The reduced stomach volume promotes earlier satiety and lower caloric intake.
ESG is an established method that can deliver significant weight loss with a lower risk profile than surgery.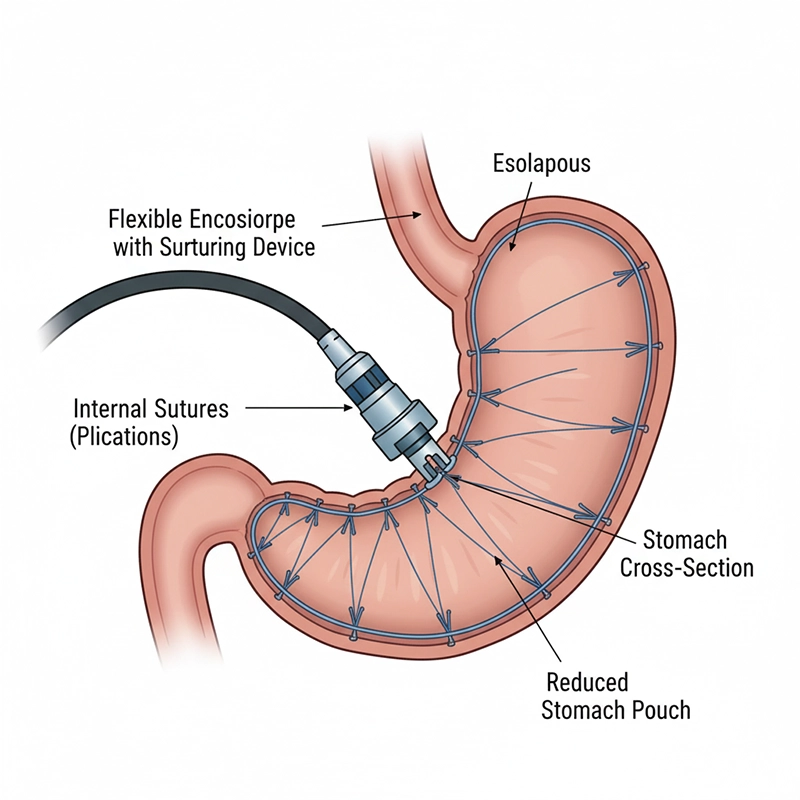
A soft, expandable balloon is placed in the stomach and filled with saline to occupy space and limit food volume.
The device is temporary (typically 6–12 months) and can be removed once treatment goals are met.
Suitable for patients seeking a reversible intervention with structured dietary support.
Endoscopic techniques can tighten or repair prior surgical alterations after weight regain.
Provides a corrective option without repeat surgery and with shorter recovery.
Helps restore treatment effectiveness while preserving natural anatomy.
Bariatric endoscopy and bariatric surgery share the goal of improving weight loss and obesity-related conditions, but endoscopic approaches offer distinct benefits that support broader access and faster recovery.
Minimally invasive: Interventions are performed internally without cutting or stapling the stomach externally, reducing tissue trauma.
Faster recovery times: Many patients go home the same day or after an overnight stay and return to normal activities within days.
Lower risk profile: Fewer complications such as infection, hernia, or deep tissue bleeding make it suitable for patients unfit for major surgery.
No external scars: Internal access avoids visible scarring and improves patient comfort.
Reversibility and flexibility: Certain options, like intragastric balloons, can be adjusted or removed to match patient progress.
Lower cost burden: Shorter stays and less intensive aftercare reduce costs for patients and healthcare providers.
These advantages explain why bariatric endoscopy is increasingly integrated into hospital treatment portfolios and promoted by medical device companies. It fills the gap between conservative therapies and surgical solutions, offering an effective balance of safety, efficiency, and accessibility.
Bariatric endoscopy is a minimally invasive medical procedure that enables physicians to perform weight loss interventions inside the stomach without external incisions. It is considered an alternative to bariatric surgery, designed for patients who struggle with obesity and require effective treatment beyond diet and exercise. Hospitals and clinics increasingly adopt bariatric endoscopy as part of their obesity management programs, offering patients faster recovery times, fewer risks, and access to advanced medical technology.
Bariatric endoscopy refers to a set of therapeutic procedures carried out with a flexible endoscope, a medical device inserted through the mouth and advanced into the stomach. The primary goal is to reduce the effective capacity of the stomach or to modify its function, helping patients achieve weight loss in a safe and controlled manner.
Unlike bariatric surgery, which involves invasive techniques such as cutting or stapling sections of the stomach, bariatric endoscopy relies on minimally invasive methods. With the support of advanced imaging and specialized instruments integrated into systems like the XBX endoscope, physicians can suture, reshape, or insert devices into the stomach while maintaining a natural anatomy.
The core principles of bariatric endoscopy include:
Minimally invasive approach: Procedures are performed without abdominal incisions.
Endoscopic visualization: Real-time imaging ensures precise control and safety.
Temporary or reversible interventions: Some methods, like intragastric balloons, can be removed once treatment goals are met.
Reduced patient burden: Shorter recovery times and fewer complications compared with surgery.
These principles position bariatric endoscopy as a practical solution for patients who are not candidates for surgery but still require effective obesity management.
Bariatric endoscopy is increasingly recommended because it bridges the gap between lifestyle modification and invasive surgery. For many patients, diet and exercise alone do not deliver sufficient weight loss, while surgery may be too risky or undesirable. Bariatric endoscopy offers a middle ground.
The main reasons to undergo bariatric endoscopy include:
Clinical necessity: It addresses obesity-related complications such as diabetes, hypertension, and sleep apnea.
Stomach volume reduction: Procedures like endoscopic sleeve gastroplasty reduce the stomach’s capacity, helping patients feel full sooner.
Safety: No external cuts or stitches, resulting in fewer risks of infection and minimal bleeding.
Faster recovery: Many patients can return to work and normal activities within a few days.
Revisional option: It can correct or adjust prior bariatric surgeries when initial results are unsatisfactory.
Healthcare efficiency: Hospitals benefit from outpatient treatment models, reducing bed occupancy and overall costs.
By combining clinical safety with patient convenience, bariatric endoscopy has become an essential tool in modern obesity treatment, supporting both individuals and healthcare providers in managing the global obesity crisis.
The process of bariatric endoscopy combines advanced imaging, precision instruments, and minimally invasive techniques to achieve meaningful weight loss. A flexible endoscope, equipped with a high-definition camera and specialized tools, is introduced through the patient’s mouth and guided down into the stomach. This enables physicians to visualize the gastrointestinal tract in real time and perform targeted procedures without the need for external incisions.
The most common bariatric endoscopic techniques include:
Endoscopic Sleeve Gastroplasty (ESG): In ESG, physicians use suturing devices attached to the endoscope to fold and stitch the stomach walls, creating a smaller, tube-like shape. This reduces the stomach’s volume, leading to earlier satiety and reduced food intake. ESG is one of the most established bariatric endoscopic methods and can result in significant weight loss with lower risk compared to surgery.
Intragastric Balloon Placement: A soft, expandable balloon is placed inside the stomach and filled with saline solution. The balloon reduces the available space for food, helping patients consume smaller portions. This method is temporary, typically lasting 6 to 12 months, after which the balloon is removed. It is suitable for patients seeking a reversible intervention.
Endoscopic Revision of Bariatric Surgery: Some patients who have undergone surgical bariatric procedures, such as gastric bypass or sleeve gastrectomy, may experience weight regain. Endoscopic revision techniques allow physicians to tighten or repair anatomical changes without repeat surgery, restoring treatment effectiveness.
The combination of these methods demonstrates the versatility of bariatric endoscopy. Whether as a primary treatment, a bridge to surgery, or a corrective intervention, the procedures are designed to be flexible and patient-centered.
One of the most important reasons bariatric endoscopy is gaining global adoption is its clinical and practical advantages over traditional surgery. While both aim to support weight loss and improve obesity-related conditions, bariatric endoscopy offers several unique benefits:
Minimally invasive: Unlike bariatric surgery, bariatric endoscopy does not involve cutting or stapling the stomach externally. All interventions are performed internally with an endoscope, reducing trauma to the body.
Faster recovery times: Most patients are discharged the same day or after an overnight stay. Normal activities can typically be resumed within a few days, compared with weeks of recovery after surgery.
Lower risk profile: Endoscopic procedures involve fewer complications such as infection, hernia, or deep tissue bleeding. This makes them suitable for patients who are not candidates for major surgery.
No external scars: Because the procedure is conducted internally, patients avoid visible scarring, an important factor for psychological comfort and post-treatment satisfaction.
Reversibility and flexibility: Some bariatric endoscopic techniques, like intragastric balloons, can be reversed or adjusted over time. This allows for personalized treatment strategies based on patient progress.
Lower cost burden: Endoscopic procedures generally require fewer hospital resources, shorter stays, and less intensive post-operative care, reducing costs for both patients and healthcare providers.
These advantages explain why bariatric endoscopy is increasingly integrated into hospital treatment portfolios and promoted by medical device companies. It fills the gap between conservative therapies and surgical solutions, offering an effective balance of safety, efficiency, and accessibility.
Bariatric endoscopy has evolved into a versatile medical solution, addressing different patient groups and clinical scenarios. Its applications extend beyond initial weight-loss interventions, making it a valuable option within modern obesity treatment programs.
Key medical indications include:
Patients not eligible for bariatric surgery: Some patients may be medically unfit for surgery due to age, comorbidities, or elevated surgical risks. Bariatric endoscopy provides these individuals with an alternative that reduces health risks while delivering effective results.
Early-stage obesity management: For patients with moderate obesity, bariatric endoscopy can serve as an early intervention. It prevents progression to more severe obesity-related complications, reducing long-term healthcare costs.
Revision after failed surgical procedures: When previous bariatric surgeries such as gastric bypass or sleeve gastrectomy result in insufficient weight loss or weight regain, endoscopic revision offers a non-surgical correction method. Physicians can adjust anatomical changes without subjecting patients to repeat surgery.
Integration into comprehensive obesity programs: Bariatric endoscopy is often combined with dietary planning, lifestyle modifications, and digital monitoring tools. Hospitals and clinics include it as part of multidisciplinary approaches, improving patient compliance and long-term outcomes.
Comorbidity management: By reducing weight, bariatric endoscopy indirectly improves obesity-related conditions such as type 2 diabetes, sleep apnea, cardiovascular disease, and hypertension. Patients benefit from holistic health improvements beyond weight control.
Because of its adaptability, bariatric endoscopy has become an integral option in both outpatient clinics and advanced hospital systems, ensuring that more patients can access treatment regardless of their surgical eligibility.
While bariatric endoscopy and bariatric surgery share the same ultimate goal—achieving significant and sustainable weight loss—they differ in methodology, risk, and patient experience. A direct comparison helps patients and healthcare providers determine the most suitable pathway.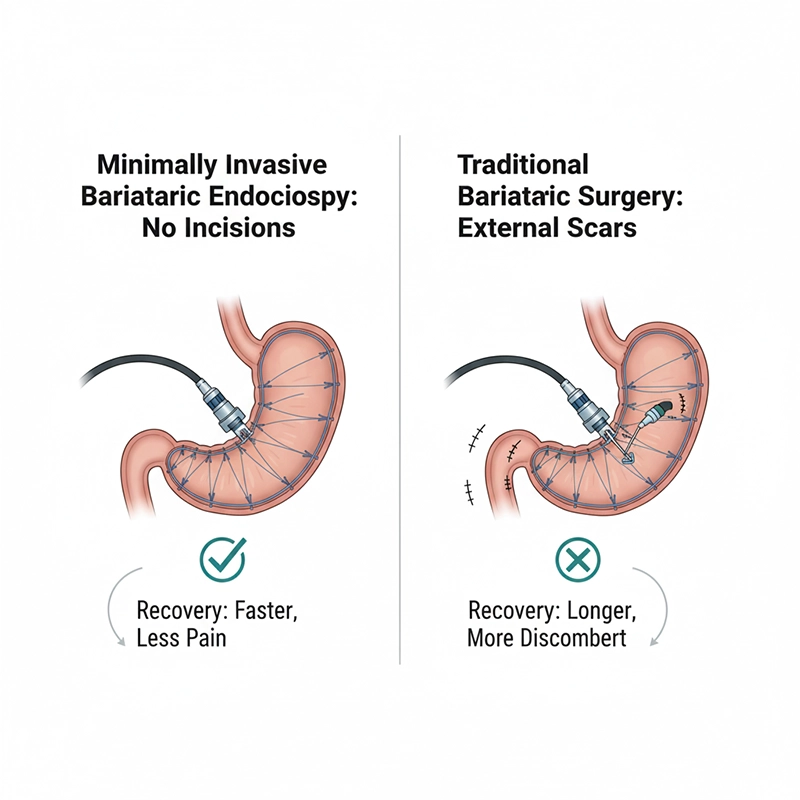
Invasiveness — Bariatric endoscopy: Minimally invasive, no external incisions. Bariatric surgery: Highly invasive, requires cutting and stapling.
Recovery time — Bariatric endoscopy: Days, often outpatient-based. Bariatric surgery: Weeks, with longer hospital stay.
Risk profile — Bariatric endoscopy: Lower risk of infection, bleeding, or complications. Bariatric surgery: Higher risk due to surgical trauma and anesthesia.
Scarring — Bariatric endoscopy: No visible scars. Bariatric surgery: Visible surgical scars.
Reversibility — Bariatric endoscopy: Some procedures reversible. Bariatric surgery: Permanent anatomical changes.
Weight loss outcomes — Bariatric endoscopy: Moderate, often 15–20% of body weight. Bariatric surgery: Significant, 25–35% of body weight or more.
Cost — Bariatric endoscopy: Lower, outpatient procedures reduce expenses. Bariatric surgery: Higher, with extended hospital resources required.
From the list, it is clear that bariatric surgery often delivers greater total weight loss, but it comes with higher risks and longer recovery. Bariatric endoscopy, on the other hand, balances safety and efficacy, making it particularly suitable for patients seeking minimally invasive options or those not eligible for major surgery.
Hospitals and procurement managers increasingly view bariatric endoscopy as a complementary approach rather than a replacement. In many cases, it serves as an entry-level treatment that can be escalated to surgery if needed, or as a secondary treatment for revising surgical outcomes. This dual role enhances its importance within modern obesity care.
Bariatric endoscopy is a minimally invasive medical procedure that enables physicians to perform weight loss interventions inside the stomach without external incisions. It is considered an alternative to bariatric surgery, designed for patients who struggle with obesity and require effective treatment beyond diet and exercise. Hospitals and clinics increasingly adopt bariatric endoscopy as part of their obesity management programs, offering patients faster recovery times, fewer risks, and access to advanced medical technology.
The global market for bariatric endoscopy is expanding rapidly, driven by rising obesity rates and the increasing demand for less invasive medical interventions. According to healthcare industry reports, obesity has reached epidemic proportions worldwide, with over 650 million adults classified as obese. This growing prevalence underscores the need for scalable, cost-effective solutions.
Several trends are shaping the market landscape:
Patients are increasingly seeking weight-loss solutions that avoid the risks of surgery. Bariatric endoscopy fulfills this need, offering outpatient-based interventions with lower complication rates.
Healthcare providers recognize bariatric endoscopy as a strategic addition to treatment portfolios. Outpatient delivery improves patient throughput, reduces costs, and aligns with preventive healthcare models.
Manufacturers such as XBX endoscope companies are investing in high-definition imaging, flexible instruments, and AI-assisted guidance systems. These innovations improve procedural safety and outcomes, fueling wider acceptance.
While bariatric endoscopy adoption began in advanced healthcare markets, developing regions are now embracing the technology. This is especially true in Asia and Latin America, where rising obesity rates demand affordable, minimally invasive interventions.
Hospitals are combining bariatric endoscopy with digital platforms for weight monitoring, telemedicine, and lifestyle coaching. This integration ensures long-term patient compliance and strengthens clinical results.
The growing demand for bariatric endoscopy reflects its role not just as a medical procedure, but as part of a global response to obesity-related health challenges.
The cost of bariatric endoscopy varies significantly depending on geographic region, healthcare system, and type of procedure performed. While it is generally more affordable than bariatric surgery, several factors influence pricing:
Endoscopic sleeve gastroplasty (ESG) is typically more expensive than intragastric balloon placement because it involves advanced suturing devices and longer procedure times.
Large hospitals with high patient volumes may offer lower costs due to economies of scale, while specialized clinics may charge premium fees for personalized care.
In North America and Western Europe, bariatric endoscopy costs range between USD 7,000 and 12,000. In contrast, procedures in Asia or Latin America may be priced 30–50% lower due to lower operational expenses.
Coverage varies by country and provider. In some regions, insurers are beginning to reimburse bariatric endoscopy as part of obesity treatment, while in others patients must pay out of pocket.
Additional expenses may include pre-procedure consultations, post-procedure dietary programs, and follow-up endoscopic evaluations. These services impact the total cost of treatment.
Compared with bariatric surgery, bariatric endoscopy is generally 30–50% less expensive. However, patients and procurement teams should weigh costs against expected outcomes. While surgery often delivers more dramatic weight reduction, bariatric endoscopy provides a safer, more affordable, and repeatable intervention.
Hospitals and procurement managers are increasingly factoring cost efficiency into their decisions, positioning bariatric endoscopy as a valuable investment for both patient health and institutional budgets.
Bariatric endoscopy equipment selection has a direct impact on procedural safety, efficiency, and long-term outcomes. Hospitals and clinics should evaluate suppliers and factories against clear technical and compliance criteria before purchase.
Procurement teams can use the following considerations to identify reliable partners and ensure clinical performance aligns with budget and risk controls.
Product quality and reliability: High-definition imaging, ergonomic handling, and robust instrument channels support complex bariatric endoscopy tasks. Suppliers such as XBX endoscope manufacturers focus on precision tools that aid consistent performance.
Certifications and compliance: Evidence of ISO 13485, CE, and comparable market clearances indicates standardized quality systems and safer manufacturing practices.
Customization and innovation: Options tailored for endoscopic sleeve gastroplasty or intragastric balloon workflows can streamline procedures and support better usability.
After-sales support: Training, maintenance plans, spare-parts availability, and responsive technical assistance reduce downtime and protect device lifespan.
Cost-effectiveness: Total cost of ownership—including service, consumables, and upgrade paths—should be weighed against performance rather than lowest unit price alone.
Balancing these factors helps hospitals select bariatric endoscopy suppliers that match clinical objectives, regulatory requirements, and financial constraints.
While bariatric endoscopy generally presents a lower risk profile than surgical alternatives, structured screening and standardized protocols remain important for patient safety.
Common side effects: Short-term nausea, vomiting, abdominal discomfort, and sore throat are typical within the first few days and are usually self-limiting with supportive care.
Serious but rare complications: Potential issues include bleeding, gastric perforation, or balloon deflation in intragastric balloon cases; early recognition and escalation pathways are essential.
Eligibility criteria: Many programs prioritize patients with BMI 30–40 who have not achieved adequate results with lifestyle therapy; higher-BMI patients may be evaluated for surgical options.
Patient adherence: Durable outcomes rely on nutrition planning, activity goals, and follow-up; without adherence, weight regain is possible regardless of technique.
Hospital risk management: Pre-procedure evaluation, informed consent, peri-procedural monitoring, and team training reduce adverse events and support consistent quality of care.
When performed by trained teams using high-quality devices and protocolized pathways, bariatric endoscopy can be delivered with a favorable safety profile and predictable operational performance.
The future of bariatric endoscopy is shaped by rapid advancements in medical technology, shifting patient expectations, and healthcare system priorities. As obesity continues to affect populations worldwide, the demand for innovative, minimally invasive interventions is expected to grow.
Enhanced suturing and closure devices:Next-generation suturing systems are being developed to increase procedural efficiency, improve durability, and minimize complications. These tools will expand the range of treatable patients and allow for more complex endoscopic reconstructions.
AI-assisted endoscopic systems:Artificial intelligence is being integrated into endoscopy platforms to improve visualization, detect complications early, and guide physician decision-making. Real-time AI assistance may enhance both safety and precision.
Digital monitoring and telemedicine integration:Post-procedure monitoring is increasingly supported by digital health platforms. Patients may use mobile apps to log dietary intake, track weight progress, and communicate with physicians remotely. This integration promotes long-term success and reduces readmission rates.
Personalized treatment pathways:Future bariatric endoscopy programs are expected to tailor interventions based on genetic, metabolic, and lifestyle factors. Customizing the approach ensures higher patient compliance and sustainable results.
Global accessibility:As medical device costs decrease and training programs expand, bariatric endoscopy will become more accessible in developing regions. This democratization of treatment is vital in addressing the global obesity crisis.
With these innovations, bariatric endoscopy is likely to evolve from a niche option to a mainstream obesity treatment, complementing surgical and lifestyle-based interventions. Hospitals that adopt these technologies early will position themselves at the forefront of obesity care.
Bariatric endoscopy represents a transformative shift in how obesity is treated across the globe. It combines the effectiveness of medical intervention with the safety and convenience of minimally invasive procedures. Patients benefit from faster recovery, fewer risks, and the possibility of reversible treatments, while hospitals and clinics gain efficiency, lower costs, and improved patient satisfaction.
From definitions and principles to applications, risks, costs, and future trends, bariatric endoscopy demonstrates its value as both a clinical and market-driven solution. With ongoing innovations from medical device suppliers such as XBX endoscope manufacturers and increasing global adoption, bariatric endoscopy is set to play a central role in the fight against obesity.
As healthcare systems seek to balance safety, affordability, and effectiveness, bariatric endoscopy provides a pathway that aligns with patient needs and institutional goals, securing its place as one of the most important developments in modern obesity treatment.
Bariatric endoscopy is a minimally invasive medical procedure performed with a flexible endoscope to reduce stomach capacity or adjust its function for weight management. It does not involve external incisions and is typically carried out in outpatient settings.
During bariatric endoscopy, an endoscope equipped with specialized tools is inserted through the mouth into the stomach. Procedures such as endoscopic sleeve gastroplasty or intragastric balloon placement reshape the stomach or reduce its volume, helping patients control food intake.
Bariatric endoscopy offers shorter recovery times, lower complication risks, and no visible scars. While surgical methods often result in greater overall weight loss, endoscopic procedures provide a safer, less invasive alternative.
Bariatric endoscopy is usually recommended for patients with a body mass index (BMI) between 30 and 40 who have not achieved sufficient results from lifestyle changes. It may also be used for patients who are not eligible for surgery due to medical risks.
Endoscopic sleeve gastroplasty is a bariatric endoscopy procedure in which sutures are placed inside the stomach to create a smaller, sleeve-like shape. This reduces the stomach’s capacity, leading to earlier satiety and reduced food intake.
Copyright © 2025.Geekvalue All rights reserved.Technical Support:TiaoQingCMS