Table of Contents
A hysteroscope is a critical diagnostic and therapeutic tool used in modern uterine health care. This medical device allows healthcare professionals to view the inside of the uterus, providing real-time visual insights essential for diagnosing and treating a range of uterine conditions. By offering precise detection and facilitating minimally invasive treatments, hysteroscopes are essential for ensuring both effective and efficient care in hospitals. Conditions such as abnormal uterine bleeding, fibroids, polyps, and infertility can be diagnosed and treated with greater accuracy and reduced recovery times compared to traditional surgical methods. The integration of hysteroscopes into routine hospital practices not only enhances the quality of care but also improves hospital efficiency by reducing the need for lengthy recovery periods and expensive surgical interventions.
A hysteroscope is a thin, lighted tube that allows doctors to look inside the uterus. The device is equipped with a camera and a light source, providing high-resolution images of the uterine lining, fallopian tubes, and cervix. Hysteroscopes are typically used for both diagnostic and therapeutic purposes. They are inserted through the vagina and cervix, providing a direct view of the uterus without the need for larger incisions.
Hysteroscopy is commonly performed in an outpatient setting, allowing patients to go home the same day. This procedure is essential for identifying a variety of uterine conditions, including:
Uterine fibroids
Polyps
Abnormal bleeding
Endometrial cancer
Infertility-related issues
1. Identifying Uterine Abnormalities
Hysteroscopy is commonly used to diagnose uterine conditions like fibroids, polyps, or endometrial cancer. It allows doctors to visually inspect the uterine lining and identify any abnormalities that may be causing symptoms such as abnormal bleeding or pain. Real-time images help doctors determine the size, shape, and location of these growths, which can then guide treatment decisions.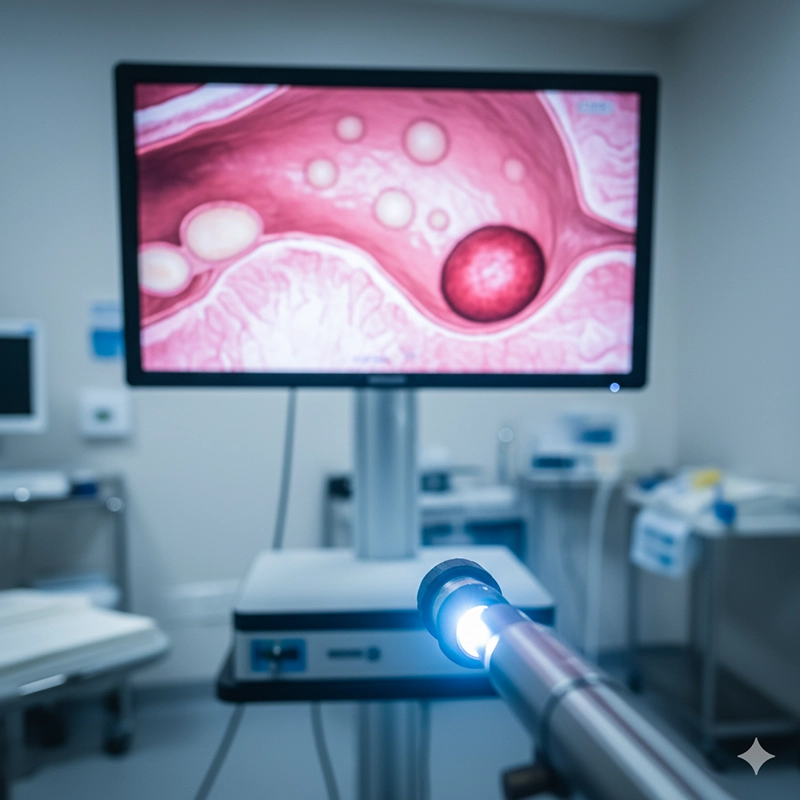
2. Investigating Infertility Issues
In cases of unexplained infertility, hysteroscopy can be used to examine the uterus for any issues that could affect implantation or fetal development. Conditions like scarring of the uterine lining (Asherman’s syndrome) or fibroids can interfere with conception. By using a hysteroscope, doctors can identify these conditions and address them early in the treatment process.
1. Removal of Uterine Polyps and Fibroids
Hysteroscopy is not only diagnostic but also therapeutic. Once a uterine abnormality such as a fibroid or polyp is identified, it can often be removed during the same procedure. This is known as operative hysteroscopy, which is less invasive than traditional surgery. The procedure significantly reduces the risk of complications, recovery times, and the need for more extensive procedures like hysterectomy.
2. Treating Abnormal Uterine Bleeding
Hysteroscopy can also be used to treat abnormal uterine bleeding. Through a procedure known as endometrial ablation, doctors can use the hysteroscope to remove or destroy the uterine lining, which is often the source of heavy bleeding. This is particularly effective for patients who do not respond well to medication or who wish to avoid a hysterectomy.
1. Reduced Recovery Time
The primary advantage of using hysteroscopes is that they are minimally invasive. Unlike traditional surgeries that require large incisions, hysteroscopic procedures are performed through the natural openings of the body—primarily the cervix. This significantly reduces the need for lengthy recovery times, enabling patients to return to their normal activities more quickly. In many cases, patients can go home the same day as the procedure.
2. Lower Risk of Complications
Since hysteroscopy requires no incisions, the risk of infection and other complications is drastically reduced. This makes it a safer alternative to traditional surgery, particularly for patients who may be at higher risk due to age or underlying health conditions. The reduced trauma to the body also lowers the chance of postoperative complications like blood clots or prolonged bleeding.
1. Real-Time Visual Insights
The hysteroscope provides real-time, high-resolution images of the uterus, making it a valuable tool for accurately diagnosing uterine conditions. This is especially beneficial in cases where other diagnostic methods, such as ultrasound or MRI, may not provide sufficient detail. By using hysteroscopy, doctors can view the uterine lining directly, allowing for more precise diagnoses and better-informed treatment decisions.
2. Immediate Treatment
One of the key advantages of hysteroscopy is that it allows for immediate treatment. If a uterine abnormality is discovered during the procedure, it can often be treated on the spot. This reduces the need for multiple visits or additional surgeries, improving patient outcomes and hospital efficiency.
1. Shorter Hospital Stays
Since hysteroscopic procedures are minimally invasive and require little to no hospitalization, hospitals can accommodate more patients and reduce overall healthcare costs. The ability to perform these procedures on an outpatient basis helps keep healthcare costs low while ensuring that patients receive high-quality care in a timely manner.
2. Streamlined Treatment Process
The integration of hysteroscopy into hospital practices allows for faster diagnosis and treatment of uterine conditions. This can reduce the need for multiple procedures or tests, saving both time and money. Additionally, because the procedure can be performed in an outpatient setting, hospitals can treat a larger volume of patients, increasing their overall efficiency.
1. Improved Imaging and Resolution
Recent advancements in hysteroscopic technology have led to significant improvements in imaging quality. Modern hysteroscopes offer HD-resolution cameras that provide clear, detailed views of the uterus, making it easier for doctors to diagnose and treat uterine conditions with greater precision. Enhanced imaging helps improve the accuracy of diagnoses and ensures that no abnormalities are missed during the procedure.
2. Integration with Other Diagnostic Tools
In addition to the improvements in imaging, modern hysteroscopes are now often integrated with other diagnostic tools such as ultrasound and biopsy equipment. This integration allows for a more comprehensive approach to uterine health care, enabling doctors to gather all the necessary information in a single visit. This also reduces the need for additional tests and follow-up visits, streamlining the entire diagnostic process.
As hysteroscopic technology continues to evolve, its role in uterine health care will likely expand even further. The introduction of robotic hysteroscopes, which offer greater precision and control, is expected to enhance the effectiveness of the procedure. Additionally, advances in imaging and artificial intelligence may allow for even more accurate diagnoses and personalized treatment plans.
In the future, hospitals that integrate these advanced technologies will be better equipped to provide high-quality, cost-effective care to their patients. The ability to diagnose and treat uterine conditions quickly and effectively will not only improve patient outcomes but also reduce the overall burden on hospital systems.
In summary, hysteroscopes are invaluable tools in modern uterine health care. They provide hospitals with the ability to diagnose and treat a wide range of uterine conditions efficiently and effectively. By reducing recovery times, lowering the risk of complications, and enabling real-time visual insights, hysteroscopy is essential for providing high-quality care to patients. As technology continues to advance, the role of hysteroscopes in uterine health care will only grow, making them an indispensable part of any modern hospital.
A hysteroscope is a thin, lighted tube with a camera that is inserted into the uterus through the cervix. It is used to diagnose and treat uterine conditions such as fibroids, polyps, abnormal bleeding, and infertility. It allows doctors to view the inside of the uterus in real-time for precise diagnosis and immediate treatment.
Hysteroscopy is a minimally invasive procedure performed through the cervix, eliminating the need for large incisions. This leads to quicker recovery times, less pain, and a lower risk of complications compared to traditional surgery, such as a hysterectomy.
Using a hysteroscope in hospitals offers several advantages: Minimally invasive: Reduces recovery time and lowers the risk of complications. Cost-effective: Minimizes hospital stays and the need for additional procedures. Real-time diagnosis and treatment: Allows for immediate action on abnormalities discovered during the procedure. Improved accuracy: Provides high-resolution, real-time images of the uterus for precise diagnosis and treatment.
Yes, hysteroscopy is generally considered a safe procedure with a low risk of complications. Because it is minimally invasive, it carries fewer risks than traditional surgeries. However, as with any medical procedure, patients should discuss any potential risks with their healthcare provider beforehand.
Copyright © 2025.Geekvalue All rights reserved.Technical Support:TiaoQingCMS