Table of Contents
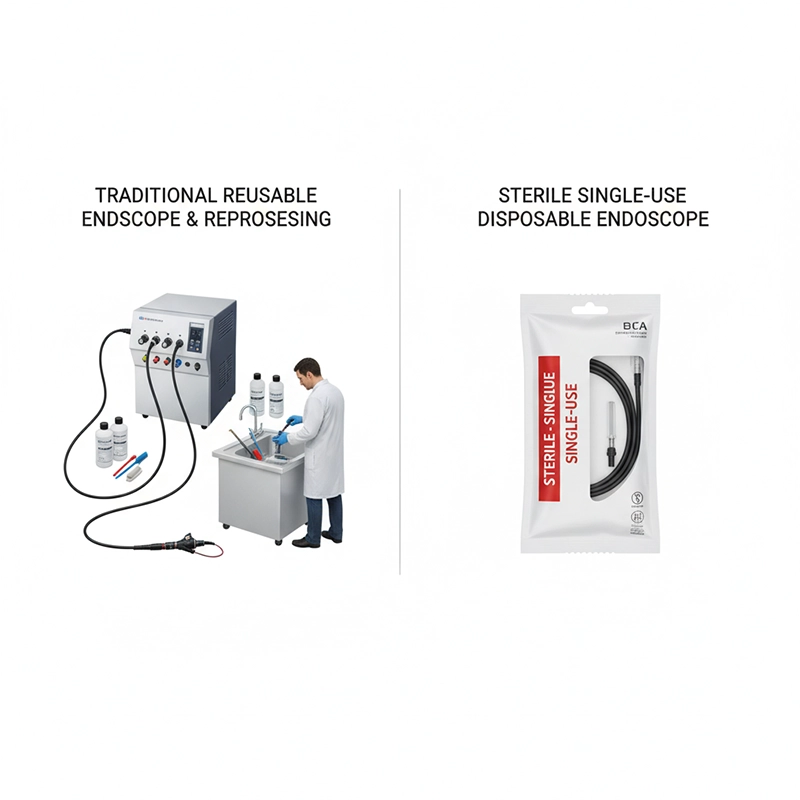
Disposable endoscopes, also known as single-use endoscopes, are medical devices designed for one-time use during diagnostic or therapeutic procedures. They are discarded immediately after use, eliminating the need for cleaning, disinfection, and reprocessing. Hospitals increasingly adopt disposable endoscopes because they provide safer, faster, and more consistent solutions in clinical practice. The shift toward disposable devices reflects a broader trend in modern healthcare: prioritizing infection control, improving workflow efficiency, and enhancing patient safety.
A disposable endoscope functions in a similar way to a traditional reusable endoscope but is optimized for single-use performance. It consists of a flexible insertion tube, an imaging system, a light source, and sometimes a working channel for instruments. The device is manufactured from lightweight polymers and integrates a CMOS digital sensor, which transmits high-quality images to a monitor or handheld display.
The principle is straightforward: the endoscope is unwrapped in sterile condition, used once for a procedure, and then safely discarded as medical waste. This design eliminates reprocessing requirements and ensures that every patient receives a device in brand-new condition.
Insertion Tube: Flexible, biocompatible polymer construction.
Imaging System: CMOS sensor at the distal tip for digital image capture.
Illumination: Built-in LED light sources for consistent visibility.
Control Section: Simplified handle for navigation and deflection.
Working Channel (optional): Allows suction, irrigation, or biopsy tools.
Connectivity: Can connect to external monitors or include built-in display units.
1. The device is inserted into the patient’s body (airway, gastrointestinal tract, urinary tract, etc.).
2. Integrated LEDs illuminate the area.
3. The CMOS chip transmits real-time images.
4. Clinicians perform diagnostic or therapeutic procedures.
5. The device is discarded after use, eliminating any possibility of cross-contamination.
This process makes disposable endoscopes highly attractive to hospitals, especially where infection control and rapid turnover are priorities.
Traditional reusable endoscopes are complex instruments with narrow channels and intricate surfaces. Even with strict cleaning and sterilization, microscopic residues may remain, creating potential risks of cross-contamination. Several studies have highlighted that infections can occur when reprocessing protocols are not followed with absolute precision.
Disposable endoscopes address this challenge by removing the need for reprocessing altogether. Since each scope is used only once, patients receive a device free from prior biological exposure. This provides hospitals with a reliable safeguard in high-risk departments such as intensive care units, emergency rooms, and oncology centers.
The Centers for Disease Control and Prevention (CDC) in the United States has reported outbreaks of multidrug-resistant organisms linked to duodenoscopes that were not fully disinfected despite adherence to reprocessing protocols.
The U.S. Food and Drug Administration (FDA) has issued safety communications acknowledging that complex reusable endoscopes may still harbor bacteria even after cleaning.
The World Health Organization (WHO) highlights infection prevention as a global priority and encourages hospitals to adopt safer technologies when feasible.
These reports do not discredit reusable endoscopes, which remain essential, but they underline why hospitals are actively exploring single-use alternatives.
Hospitals operate under pressure to balance safety, efficiency, and cost-effectiveness. Disposable endoscopes offer clear advantages:
Faster Turnover: No waiting for cleaning or sterilization between cases.
Lower Resource Burden: Less dependence on central sterile processing departments.
Flexibility in Emergencies: Devices are always available in sealed sterile packaging.
Cost Transparency: Predictable per-procedure cost with no repair or maintenance fees.
Support for Smaller Facilities: Clinics without reprocessing equipment can still provide high-quality endoscopic care.
These features align with the operational realities of modern hospitals, where both time and patient safety are critical.
From the patient’s perspective, disposable endoscopes deliver several tangible benefits:
Reduced Infection Risk: Patients face minimal risk of exposure to pathogens from prior procedures.
Shorter Waiting Times: Faster case turnover means earlier diagnosis and treatment.
Immediate Access in Emergencies: Critical in airway obstruction, gastrointestinal bleeding, or other urgent conditions.
Consistent Device Quality: Each procedure uses a brand-new instrument with no wear or degradation.
Improved Comfort: Lighter and slimmer disposable designs can reduce discomfort.
Psychological Assurance: Patients feel reassured knowing the scope is sterile and has never been used before.
A 2019 FDA review found that some duodenoscopes retained contamination despite proper cleaning, leading to infections; disposable models were recommended in high-risk cases.
A 2021 study in The Lancet Respiratory Medicine showed disposable bronchoscopes reduced delays in intensive care units, improving outcomes.
European Society of Gastrointestinal Endoscopy (ESGE) guidelines acknowledge disposable devices as effective in patient groups with elevated infection risk.
Both disposable and reusable endoscopes play important roles in modern healthcare. Many hospitals adopt a hybrid model, using disposable scopes in high-risk or high-turnover cases while keeping reusable ones for complex, long-duration interventions.
| Aspect | Reusable Endoscopes (Traditional) | Disposable Endoscopes (Single-Use) |
|---|---|---|
| Infection Safety | Relies on meticulous reprocessing; risk minimized when protocols followed | Zero risk of cross-contamination from prior patients |
| Image & Optics Quality | Advanced optics with superior resolution for complex cases | Modern CMOS delivers reliable resolution for most procedures |
| Cost Consideration | High upfront investment; cost-effective with large volumes | Predictable per-use cost; avoids repair/sterilization fees |
| Availability | May be delayed due to reprocessing requirements | Always ready, sterile, ideal for emergencies |
| Procedure Scope | Supports complex and specialized interventions | Suitable for standard diagnostic and therapeutic cases |
| Patient Benefit | Trusted in advanced, long-duration treatments | Lower infection risk, shorter waits, consistent quality |
| Environmental Aspect | Less waste, but consumes water, detergents, and energy for reprocessing | Generates waste, but avoids chemical and energy use for cleaning |
This balanced comparison shows that both disposable and reusable endoscopes have their own strengths. Hospitals are increasingly adopting a hybrid model, selecting disposable devices for infection-sensitive or emergency cases, while relying on reusable systems for complex, long-duration procedures. This approach maximizes safety, efficiency, and patient outcomes without compromising flexibility.
The global market for disposable endoscopes has expanded rapidly over the past decade. Several drivers explain this momentum:
Rising Awareness of Infection Control: Hospitals and regulators continue to emphasize patient safety, encouraging the adoption of single-use devices.
Technological Advances: Improvements in CMOS sensors, polymer materials, and LED lighting have enabled high-quality imaging at lower manufacturing costs.
Shift Toward Outpatient and Ambulatory Care: Clinics and day-surgery centers without full reprocessing infrastructure are adopting disposable devices to expand service offerings.
Regulatory Encouragement: Agencies such as the FDA and European authorities have issued guidance supporting single-use solutions in high-risk situations.
Investment by Leading Companies: Manufacturers are increasing R&D to deliver specialized disposable endoscopes for gastroenterology, urology, pulmonology, gynecology, and orthopedics.
Analysts forecast that by 2025, the disposable endoscope market will reach several billion USD globally, with the highest adoption rates in North America, Europe, and rapidly growing uptake in Asia-Pacific hospitals.
The financial implications of disposable endoscope adoption vary depending on hospital size, procedure volume, and local labor costs.
Cost Perspective: While reusable endoscopes appear cost-efficient over many cycles, they require high capital investment, reprocessing equipment, maintenance, and repair. Disposable endoscopes eliminate these hidden costs but introduce predictable per-use expenses.
Efficiency Perspective: Disposable devices save significant staff time by avoiding sterilization. Hospitals with limited workforce capacity often find the time savings outweigh per-unit costs.
Sustainability Perspective: The debate on environmental impact remains ongoing. Reusable devices generate less physical waste but require chemicals, detergents, and energy for reprocessing. Disposable devices create waste but avoid chemical use. Manufacturers are increasingly exploring recyclable materials and eco-friendly disposal methods.
Hospitals therefore evaluate both direct financial costs and indirect efficiency gains when considering disposable adoption.
As adoption grows, hospital procurement teams face the challenge of selecting reliable suppliers. Choosing the right disposable endoscope manufacturers is critical to balancing cost, safety, and long-term value.
Product Quality: Compliance with international standards such as FDA approval or CE marking.
Range of Devices: Availability of specialized models (bronchoscope, hysteroscope, cystoscope, etc.) for different departments.
Technical Support: Access to training, troubleshooting, and clinical integration support.
Pricing and Contracts: Transparent per-unit pricing, with options for bulk purchasing.
Innovation and R&D: Commitment to continuous improvement, especially in image quality and ergonomics.
Supply Chain Reliability: Consistent delivery timelines, critical for high-volume hospitals.
Hospitals increasingly prefer manufacturers that offer customized procurement solutions, including volume-based contracts, integrated monitor systems, and training programs for clinical staff.
Beyond general advantages, each category of disposable endoscope serves distinct clinical needs. Hospitals evaluate these devices according to specialty requirements.
Setting: Pulmonology, intensive care, emergency departments.
Use: Airway visualization, suction, secretion sampling, foreign body removal.
Conditions: Pneumonia, COPD, lung tumors, airway bleeding.
Setting: Gynecology clinics, outpatient surgery.
Use: Inserted via cervix for uterine visualization, minor interventions.
Conditions: Endometrial polyps, fibroids, infertility diagnosis, abnormal bleeding.
Setting: Gastroenterology, colorectal surgery.
Use: Inserted via rectum to visualize the colon; allows biopsy and polypectomy.
Conditions: Colorectal cancer screening, IBD, polyps.
Setting: Urology departments.
Use: Introduced via urethra into bladder or ureters.
Conditions: Bladder tumors, urinary stones, hematuria.
Setting: Gastroenterology.
Use: Inserted orally for stomach visualization, biopsy, or therapeutic intervention.
Conditions: Gastritis, ulcers, upper GI bleeding, early gastric cancer.
Setting: ENT, anesthesiology.
Use: Inserted via mouth to visualize larynx; crucial for airway management.
Conditions: Vocal cord lesions, laryngeal cancer, emergency intubation.
Setting: Orthopedics, sports medicine.
Use: Inserted via small incision into joint cavity, supports minimally invasive repair.
Conditions: Meniscus tears, ligament injuries, arthritis.
| Disposable Endoscope | Clinical Department | Primary Use | Typical Conditions |
|---|---|---|---|
| Bronchoscope | Pulmonology, ICU | Airway visualization, suction, sampling | Pneumonia, COPD, airway bleeding, tumors |
| Hysteroscope | Gynecology | Uterine visualization and minor procedures | Polyps, fibroids, infertility evaluation |
| Colonoscope | Gastroenterology | Colon visualization, biopsy, polypectomy | Colorectal cancer, IBD, polyps |
| Cystoscope / Ureteroscope | Urology | Bladder/ureter visualization, interventions | Stones, bladder tumor, hematuria |
| Gastroscope | Gastroenterology | Stomach visualization and biopsy | Gastritis, ulcers, GI bleeding |
| Laryngoscope | ENT, Anesthesiology | Larynx visualization, intubation | Vocal cord disease, laryngeal cancer, obstruction |
| Arthroscope | Orthopedics | Joint visualization and minimally invasive repair | Meniscus tear, ligament injury, arthritis |
 Future Outlook for Disposable Endoscopes in Hospitals
Future Outlook for Disposable Endoscopes in HospitalsLooking ahead, disposable endoscopes are expected to play an increasingly significant role in healthcare systems worldwide. Several trends will shape their future:
Broader Clinical Acceptance: More specialties are integrating single-use devices into standard practice.
Improved Imaging: Ongoing R&D will close the gap between disposable and high-end reusable scopes.
Sustainability Solutions: Manufacturers are investing in recyclable materials and eco-friendly disposal programs.
Hybrid Hospital Models: Hospitals will continue to combine disposable and reusable scopes, applying each where they are most effective.
Global Accessibility: Disposable devices will expand access to advanced procedures in regions with limited infrastructure, improving global health equity.
The trajectory is clear: disposable endoscopes will not replace reusable ones entirely, but they will become a permanent and indispensable complement in modern hospitals. Their adoption is no longer a matter of “if,” but “how extensively.”
Yes. Manufacturers can provide disposable endoscope models designed for gastroenterology, pulmonology, gynecology, urology, and orthopedics, each optimized for its intended use.
Disposable endoscopes have predictable per-unit pricing and eliminate costs for reprocessing, repairs, and maintenance, making them cost-effective in high-turnover or high-risk departments.
Most disposable endoscopes are built with biocompatible polymers, integrated CMOS imaging sensors, and LED light sources to balance safety, performance, and affordability.
Yes. Depending on the model, disposable endoscopes can include working channels for biopsy, irrigation, and suction, similar to reusable models.
After use, disposable endoscopes should be handled as regulated medical waste, following local hospital infection control and disposal guidelines.
Copyright © 2025.Geekvalue All rights reserved.Technical Support:TiaoQingCMS