جدول المحتويات
تنظير المعدة، المعروف أيضًا باسم تنظير الجهاز الهضمي العلوي، هو إجراء طبي طفيف التوغل يتيح التصوير المباشر للجهاز الهضمي العلوي، بما في ذلك المريء والمعدة والجزء الأول من الأمعاء الدقيقة (الاثني عشر). يُجرى هذا الإجراء باستخدام أنبوب مرن يُسمى منظار المعدة، وهو مزود بكاميرا عالية الدقة ومصدر ضوء. الغرض الرئيسي من تنظير المعدة هو تشخيص، وأحيانًا علاج، أمراض الجهاز الهضمي، وتوفير صور آنية أكثر دقة من وسائل التصوير الأخرى مثل الأشعة السينية أو التصوير المقطعي المحوسب.
يُستخدم تنظير المعدة على نطاق واسع في المستشفيات والعيادات ومراكز أمراض الجهاز الهضمي المتخصصة لأغراض التشخيص والعلاج. يتيح هذا الفحص تحديد حالات مثل التهاب المعدة، وقرحة المعدة، والسلائل، والأورام، والسرطانات في مراحلها المبكرة، كما يمكن أخذ خزعات من الأنسجة للتحليل النسيجي. تستغرق العملية عادةً من 15 إلى 30 دقيقة، حسب درجة تعقيدها، وتُعتبر آمنة وقليلة المخاطر.
لقد كان تطور تنظير المعدة على مدى العقود الماضية مدفوعًا بالتقدم في التكنولوجيا، بما في ذلك التصوير عالي الدقة، والتصوير ضيق النطاق، والتكامل مع الذكاء الاصطناعي (AI)، مما يساعد الأطباء على اكتشاف التغيرات المخاطية الدقيقة وتحسين دقة التشخيص.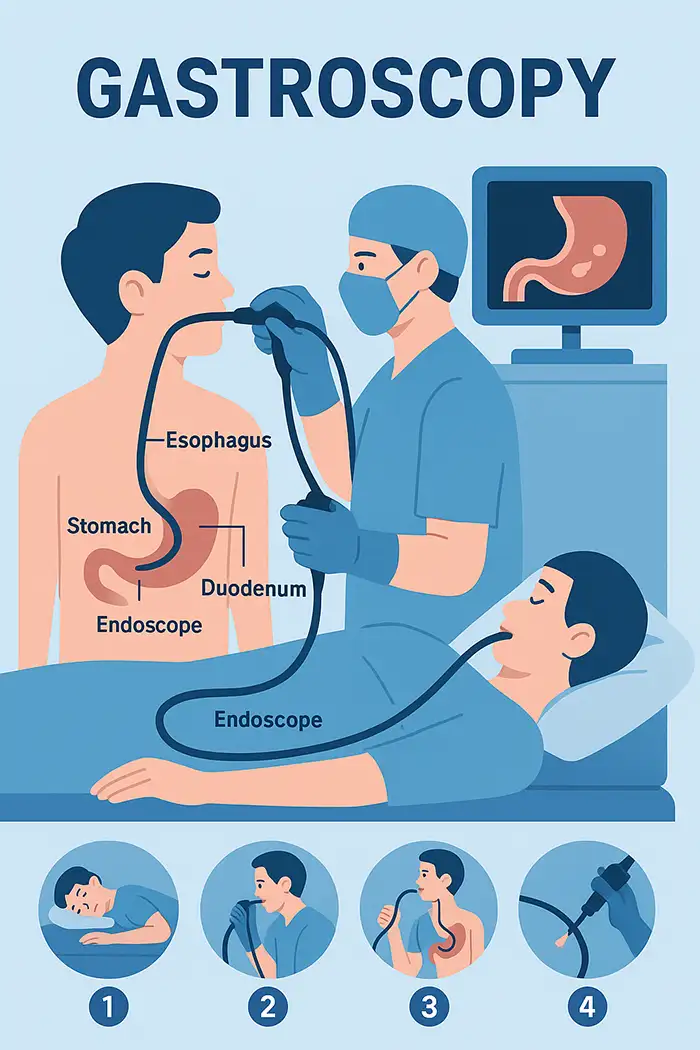
يوفر تنظير المعدة رؤية مباشرة للمريء والمعدة والاثني عشر.
إنه يكتشف الحالات التي لا يمكن رؤيتها من خلال التصوير القياسي، مثل التهاب المعدة، والقرحة، ومريء باريت، أو سرطان المعدة في مرحلة مبكرة.
يسمح بالتقييم التشخيصي والتدخلات العلاجية في وقت واحد.
مهم للمرضى الذين يعانون من آلام مستمرة في الجزء العلوي من البطن، أو نزيف معدي معوي غير مبرر، أو ارتجاع مزمن.
يتيح أخذ خزعات الأنسجة للتقييم النسيجي المرضي، وهو أمر بالغ الأهمية لتشخيص عدوى الجرثومة الملوية البوابية، أو مرض الاضطرابات الهضمية، أو الأورام المبكرة.
يدعم الطب الوقائي من خلال تحديد الآفات السرطانية في وقت مبكر.
يقلل من الحاجة إلى زيارات متعددة ويسمح بالتدخل الفوري.
تحسين رعاية المرضى والكشف المبكر ونتائج العلاج.
أنبوب مرن مع كاميرا عالية الدقة ومصدر ضوء.
تسمح القنوات العاملة بأخذ الخزعة، وإزالة الزوائد اللحمية، وإيقاف النزيف، أو علم الخلايا.
الميزات المتقدمة: التصوير ضيق النطاق، التكبير، التنظير الكروموسومي، التعزيز الرقمي.
يدعم تسجيل وتخزين الفيديو في الوقت الفعلي للتوثيق أو الطب عن بعد.
يستلقي المريض على جانبه الأيسر، ويتم تطبيق التخدير الموضعي أو المهدئ الخفيف.
منظار المعدة يتم إدخاله عن طريق الفم، ويمر عبر المريء والمعدة والاثني عشر.
يتم فحص الغشاء المخاطي بحثًا عن أي تشوهات، ويتم إجراء خزعات أو تدخلات علاجية إذا لزم الأمر.
يتم عرض الصور على شاشة عالية الدقة للتوثيق.
يقوم بتقييم النزيف في الجهاز الهضمي العلوي وتحديد مواقع العلاج.
يتم فحص المرضى المعرضين للخطر للكشف عن التغيرات السرطانية المبكرة.
يقوم بمراقبة الحالات المزمنة مثل مريء باريت.
يتم دمجها مع خزعة أو فحوصات الدم أو اختبار الجرثومة الملوية البوابية للحصول على رعاية شاملة.
ألم مستمر في الجزء العلوي من البطن أو عسر الهضم.
الكشف عن قرحة المعدة أو الاثني عشر المسببة للنزيف أو الانسداد.
تقييم النزيف المعوي (القيء الدموي أو البراز الأسود).
مراقبة التهاب المعدة أو التهاب المريء أو مريء باريت.
تشخيص الإصابة بالجرثومة الملوية البوابية.
فحص سرطان المعدة والمريء لدى المرضى المعرضين للخطر.
الكشف المبكر عن خلل التنسج أو الأورام الغدية.
تصنيف المخاطر حسب العوامل المرتبطة بأسلوب الحياة (الكحول، التدخين، النظام الغذائي).
المراقبة بعد الجراحة أو العلاج في المعدة.
الفحص الروتيني للمرضى الذين تزيد أعمارهم عن 50 عامًا أو في المناطق ذات الانتشار العالي.
الصيام لمدة 6-8 ساعات للتأكد من أن المعدة فارغة.
قم بتعديل أدوية تسييل الدم إذا لزم الأمر.
تقديم التاريخ الطبي الكامل بما في ذلك الحساسية وردود الفعل التخديرية السابقة.
تجنب التدخين والكحول وبعض الأدوية قبل الإجراء.
شرح الإجراء والغرض والمخاطر والنتائج المتوقعة.
معالجة القلق أو الخوف من الأماكن المغلقة.
الحصول على الموافقة المستنيرة لأغراض التشخيص والعلاج.
ترتيب النقل بعد العملية إذا تم استخدام التخدير.
المراقبة المستمرة للعلامات الحيوية.
الفحص المنهجي لتجنب تفويت الآفات الدقيقة.
يتم جمع الخزعات وإجراء الإجراءات العلاجية إذا لزم الأمر.
تم توثيق النتائج غير الطبيعية، وتم تخزين الصور/الفيديو للسجلات.
يعد الضغط الخفيف أو الانتفاخ أو التهاب الحلق أمرًا شائعًا ولكنه مؤقت.
يساعد التخدير أو التخدير الموضعي على تقليل الشعور بعدم الراحة.
تستغرق الإجراءات من 15 إلى 30 دقيقة؛ والتعافي خلال 1 إلى 2 ساعة.
استأنف أنشطتك الطبيعية تدريجيًا؛ واتبع نصائح النظام الغذائي والترطيب.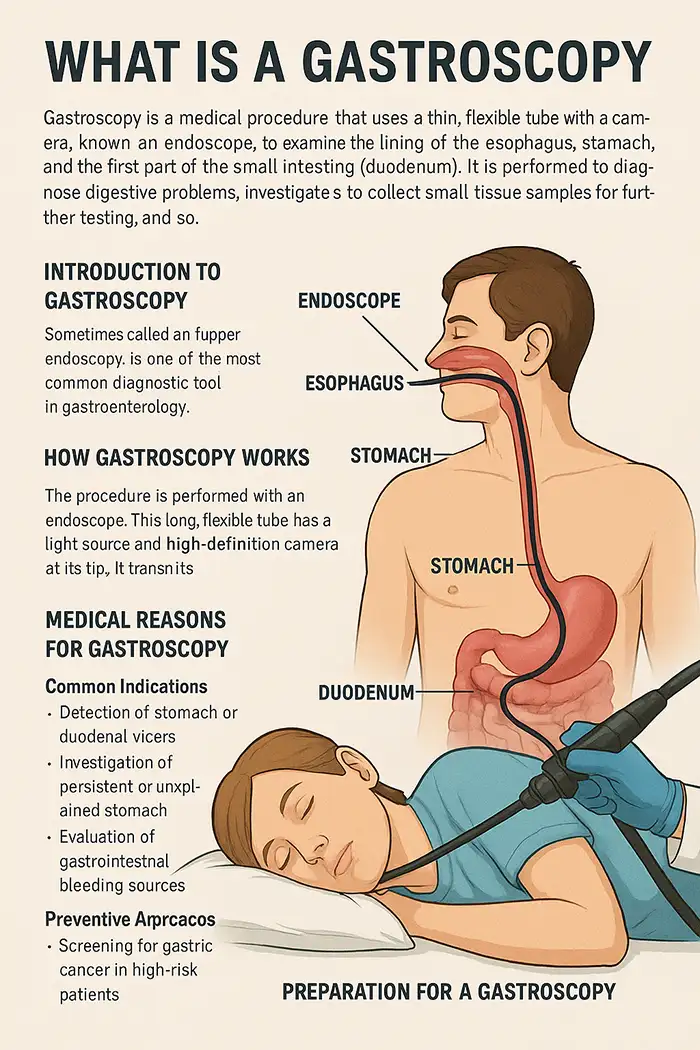
يعتمد الألم على التخدير، ومنعكس البلع، ومدة الإجراء، والتشريح.
عادة ما يشعر المرضى الذين يخضعون للتخدير بأقل قدر من الانزعاج.
تعمل بخاخات أو جل التخدير الموضعي على تقليل رد الفعل المنعكس للبلعوم.
يضمن التخدير الوريدي الخفيف الاسترخاء.
تساعد تقنيات التنفس والاسترخاء على الشعور بالراحة.
تساعد التقنية اللطيفة التي يقدمها أخصائي التنظير ذو الخبرة على تقليل التوتر.
تهيج أو وجع بسيط في الحلق.
خطر حدوث نزيف الخزعة ضئيل، وعادة ما يختفي تلقائيًا.
نادرة: ثقب، أو عدوى، أو رد فعل مهدئ.
يحتاج مرضى أمراض القلب والرئة الشديدة إلى مراقبة إضافية.
التعقيم الصارم للمناظير.
يتم مراقبة التخدير من قبل الموظفين المدربين.
بروتوكولات الطوارئ جاهزة للمضاعفات.
تدريب الموظفين بشكل منتظم على السلامة ورعاية المرضى.
التهاب المعدة، التهاب المريء، التهاب الغشاء المخاطي، قرحة المعدة.
مصادر النزيف المعدي المعوي، الاورام الحميدة، الاورام، عدوى الجرثومة الملوية البوابية.
الآفات السرطانية السابقة، مريء باريت، سرطان المعدة المبكر.
الحالات المزمنة: التهاب المعدة المتكرر، الارتجاع، التغيرات بعد الجراحة.
التشوهات التشريحية: التضيقات، فتق الحجاب الحاجز.
الأشعة السينية: منظر هيكلي، بدون خزعة.
التصوير المقطعي المحوسب: صور مقطعية، تفاصيل مخاطية محدودة.
تنظير الكبسولة: يصور الأمعاء الدقيقة ولكن بدون خزعة/تدخل.
التصور المباشر، إمكانية أخذ الخزعة، الكشف المبكر عن الآفة، التدخلات العلاجية.
يقلل الحاجة إلى زيارات تشخيصية متعددة.
يتيح العلاج بأقل قدر من التدخل الجراحي.
المراقبة حتى زوال تأثير التخدير (30-60 دقيقة).
الأطعمة اللينة والترطيب في البداية.
عادةً ما يختفي الانتفاخ الخفيف أو الغازات أو انزعاج الحلق بسرعة.
أبلغ فورًا عن أي ألم شديد في البطن أو قيء أو نزيف.
مراجعة نتائج الخزعة وإدارة المتابعة.
المراقبة الدورية للحالات المزمنة أو ما بعد العلاج.
التصوير عالي الدقة، والتصوير ضيق النطاق، والتنظير الكروموسومي، والتصور ثلاثي الأبعاد لاكتشاف الآفات بشكل أفضل.
يساعد الكشف بمساعدة الذكاء الاصطناعي على تقليل الخطأ البشري ويدعم التشخيص في الوقت الفعلي.
يساعد الذكاء الاصطناعي في التدريب من خلال تسليط الضوء على المناطق المشبوهة لأخصائيي التنظير الداخلي الجدد.
استئصال الغشاء المخاطي بالمنظار لإزالة الورم في وقت مبكر دون جراحة.
تساعد تقنيات وقف النزيف على السيطرة على النزيف بشكل فعال.
تتيح الأجهزة المتقدمة التدخلات الأقل تدخلاً لعلاج السلائل والتضيقات.
تقييم القطر والمرونة ودقة التصوير.
خذ في الاعتبار سمعة المورد والشهادات وجودة الخدمة.
ضمان التوافق مع أدوات الخزعة والشفط والعلاج.
تحقيق التوازن بين التكلفة والجودة للحصول على أقصى قيمة سريرية.
خذ بعين الاعتبار الضمان والصيانة ودعم التدريب.
الشراء بالجملة مقابل الشراء بوحدة واحدة بناءً على الطلب السريري.
يُعدّ تنظير المعدة أداةً لا غنى عنها في طب الجهاز الهضمي الحديث، إذ يجمع بين دقة التشخيص والفحص الوقائي والقدرة العلاجية. إن قدرته على تصوير الجهاز الهضمي العلوي مباشرةً، وأخذ الخزعات، والكشف المبكر عن الآفات، تجعله بالغ الأهمية في كلٍّ من الرعاية الروتينية ومراقبة المرضى المعرضين لمخاطر عالية. وقد عززت التطورات التكنولوجية، مثل التصوير عالي الدقة، والتصوير ضيق النطاق، والكشف بمساعدة الذكاء الاصطناعي، دقة التشخيص وراحة المريض. كما يضمن التحضير الجيد، وبروتوكولات السلامة، والرعاية بعد العملية نتائج مثالية. ويُحسّن اختيار معدات عالية الجودة وموردين موثوقين الكفاءة والسلامة ورعاية المرضى. ويظل تنظير المعدة في طليعة تشخيصات الجهاز الهضمي قليلة التوغل، حيث يلعب دورًا حاسمًا في التدخل المبكر، والطب الوقائي، وتحسين جودة حياة المريض.
يمكن للمستشفيات الاختيار من بين مناظير المعدة التشخيصية القياسية، ومناظير المعدة العلاجية ذات قنوات العمل الأكبر، والنماذج المتقدمة التي تتميز بالتصوير عالي الدقة أو التصوير ضيق النطاق.
يجب أن تتوافق جميع أجهزة تنظير المعدة مع شهادات ISO وCE، ويجب على الموردين تقديم تقارير ضمان الجودة، والتحقق من التعقيم، ووثائق الامتثال التنظيمي.
نعم، تتضمن المناظير المعدية الحديثة قنوات عمل لملاقط الخزعة، وأدوات إزالة الزوائد اللحمية، وأجهزة وقف النزيف، مما يسمح بإجراءات تشخيصية وعلاجية.
يوصى باستخدام التصوير عالي الدقة والتصوير ضيق النطاق والتنظير الكروموسومي الرقمي للكشف عن التغيرات المخاطية الدقيقة وتحسين دقة التشخيص.
توفر معظم الموردين ضمانًا لمدة تتراوح من سنة إلى ثلاث سنوات، والصيانة الوقائية، والدعم الفني في الموقع، وتوافر قطع الغيار لضمان الموثوقية على المدى الطويل.
نعم، تدعم العديد من أجهزة التنظير المتقدمة تسجيل الفيديو الرقمي وتخزينه ودمجه مع أنظمة PACS أو منصات الطب عن بعد للاستشارة عن بعد.
إن بروتوكولات التعقيم المناسبة، والتخدير الخاضع للمراقبة، والموظفين المدربين على إجراءات الطوارئ ضرورية لضمان سلامة المرضى والامتثال لمعايير المستشفى.
غالبًا ما يقدم الموردون التدريب في الموقع، وأدلة المستخدم، والبرامج التعليمية الرقمية، وقد يقدمون ورش عمل للتقنيات المتقدمة مثل التنظير بمساعدة الذكاء الاصطناعي.
تشمل الملحقات الشائعة ملقط الخزعة، وفرش الخلايا، وإبر الحقن، وفرش التنظيف، وواقيات الفم التي تستخدم لمرة واحدة لراحة المريض والسيطرة على العدوى.
يجب على فرق المشتريات مقارنة مواصفات المعدات، ودعم ما بعد البيع، وشروط الضمان، وخدمات التدريب، واختيار الموردين ذوي الخبرة السريرية المثبتة والامتثال للشهادات.
جميع الحقوق محفوظة © 2025.Geekvalue.الدعم الفني: TiaoQingCMS