Table of Contents
Upper endoscopy is a medical procedure that allows doctors to examine the esophagus, stomach, and duodenum using a flexible, camera-equipped tube. It helps diagnose digestive issues, detect abnormalities, and guide treatment in a minimally invasive way.
Upper endoscopy, also known as esophagogastroduodenoscopy (EGD), is a cornerstone diagnostic and therapeutic tool in modern gastroenterology. It involves inserting a thin, flexible tube equipped with a light and high-resolution camera through the patient’s mouth, passing down the esophagus, into the stomach, and reaching the duodenum. The ability to visualize the mucosal surfaces directly provides physicians with unparalleled diagnostic accuracy, while accessory channels enable therapeutic interventions during the same session.
The relevance of upper endoscopy continues to grow as digestive disorders such as gastroesophageal reflux disease (GERD), ulcers, gastrointestinal bleeding, and cancers rise globally. It represents a bridge between non-invasive imaging and open surgical approaches, offering both clarity and patient safety.
The concept of visualizing the gastrointestinal tract dates back centuries, but modern upper endoscopy became possible with technological innovations in optics and illumination. Early rigid scopes in the 19th century gave way to semi-flexible devices in the early 20th century, but it was not until the 1950s and 1960s that flexible fiber-optic endoscopes revolutionized the field.
With the later integration of charge-coupled devices (CCD) and complementary metal-oxide semiconductor (CMOS) sensors, endoscopes became capable of high-definition imaging, digital recording, and integration with computer systems. Recent advancements such as narrow band imaging (NBI), magnification endoscopy, and artificial-intelligence–assisted analysis are expanding its diagnostic accuracy even further.
Direct visualization of the esophagus, stomach, and duodenum.
Biopsy sampling to detect infections, inflammation, or cancer.
Therapeutic procedures such as polyp removal, dilation, and treatment of bleeding.
Support for screening programs in populations at risk of gastric or esophageal cancer.
Reduced need for exploratory surgery and shorter hospital stays with cost-effective accuracy.
Persistent heartburn or acid reflux unresponsive to medication
Difficulty swallowing (dysphagia)
Upper gastrointestinal bleeding (hematemesis or melena)
Chronic nausea, vomiting, or unexplained abdominal pain
Anemia caused by gastrointestinal blood loss
Suspicion of gastric or esophageal tumors
Unexplained weight loss or malnutrition
Removal of polyps or foreign bodies
Dilation of strictures or narrowed segments
Treatment of bleeding with cauterization, clipping, or banding
Placement of feeding tubes or stents
Localized drug delivery, such as steroid injections
Fasting for 6–8 hours before the procedure to ensure an empty stomach
Reviewing medical history, allergies, and current medications
Stopping certain medications (e.g., anticoagulants) if advised by a doctor
Explaining sedation options and obtaining informed consent
Intravenous sedation is typically administered to relax and minimize discomfort
A local anesthetic spray may be applied to the throat
Continuous monitoring of vital signs ensures safety throughout the examination
Sedation and Positioning – The patient lies on their left side, and sedation is administered.
Insertion of the Endoscope – The endoscope is gently advanced through the mouth, pharynx, and esophagus.
Examination of the Esophagus – Doctors check for reflux esophagitis, strictures, or varices.
Visualization of the Stomach – Gastritis, ulcers, or tumors can be identified.
Inspection of the Duodenum – Conditions such as duodenitis, celiac disease, or early cancers may be detected.
Biopsy or Treatment – Tissue samples may be taken, or therapeutic interventions performed.
Withdrawal and Monitoring – The endoscope is withdrawn slowly, ensuring a final inspection of all structures.
The entire procedure typically lasts between 15 and 30 minutes, with recovery in a short-stay unit afterward.
Mild sore throat or bloating after the procedure
Adverse reactions to sedation
Bleeding from biopsy or treatment sites
Rare perforation of the gastrointestinal tract
Infection (extremely rare with modern sterilization)
Most complications are rare, occurring in less than 1% of cases, and are manageable with prompt medical care.
Patients rest until the sedative wears off and should not drive or operate machinery for 24 hours
Mild throat discomfort is common but temporary
Biopsy results may take a few days; clinicians then discuss findings and treatment plans
Flexible insertion tube that enhances maneuverability and comfort
Light source (LED or xenon) for bright illumination
High-definition imaging system capturing real-time visuals
Accessory channels for biopsy, suction, and therapeutic tools
Processor and monitor for display, recording, and digital storage
Innovations such as disposable endoscopes, capsule endoscopy, and AI-assisted analysis are shaping the future. Manufacturers continually enhance ergonomics, resolution, and safety to meet the demands of modern hospitals.
Emergency care – management of bleeding ulcers or varices
Outpatient clinics – diagnosis of chronic reflux or dyspepsia
Cancer screening programs – early detection of gastric or esophageal cancers
Post-surgical follow-up – evaluating healing or complications
By providing real-time data, upper endoscopy reduces diagnostic uncertainty and helps guide immediate treatment.
The demand for upper endoscopy equipment is increasing worldwide due to rising gastrointestinal disease prevalence, aging populations, and expanded screening programs.
Technological innovation – improved imaging and AI tools
Hospital modernization – need for advanced diagnostic devices
Preventive healthcare – emphasis on early detection
OEM/ODM production – allowing hospitals to customize devices to their needs
Procurement teams often evaluate endoscope manufacturers based on quality, certifications, after-sales support, and scalability.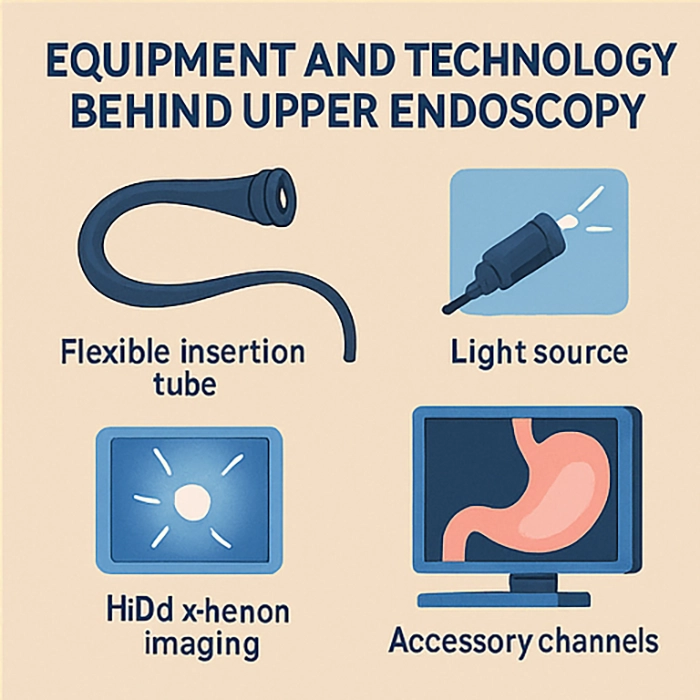
In the competitive field of medical technology, companies such as XBX play a pivotal role. XBX provides hospital-grade endoscopy systems with options for customization through OEM and ODM services. By focusing on high-definition imaging, ergonomic design, and global certifications, XBX supports hospitals in upgrading their diagnostic capacity.
Flexible procurement models for bulk or tailored orders
Strong quality assurance with international certifications
Technical support and training for hospital staff
Innovation-driven development with advanced imaging technology
Through strategic procurement from trusted suppliers, hospitals can secure reliable and cost-effective upper endoscopy systems.
Artificial intelligence – real-time lesion detection and diagnostic support
Virtual endoscopy – combining imaging with 3D modeling
Robotics – enhancing precision and reducing operator fatigue
Single-use endoscopes – improving infection control
Integrated data systems – connecting endoscopy findings with electronic health records
These innovations will further cement upper endoscopy as a cornerstone of gastroenterology and preventive healthcare.
Upper endoscopy provides a safe, effective, and versatile method to diagnose and treat upper gastrointestinal conditions. From its historical roots to the latest AI-driven systems, it continues to evolve with medicine’s growing demands. Hospitals worldwide rely on its ability to provide direct visualization, immediate interventions, and reliable results. With the support of innovative suppliers like XBX, healthcare systems can ensure patients benefit from the highest standards of diagnostic care.
Upper endoscopy systems can be supplied in HD or 4K imaging, with options for single-channel or dual-channel scopes, advanced illumination, and integration with hospital IT systems.
Yes, many manufacturers including XBX offer OEM/ODM services, allowing customization in scope diameter, ergonomic handle design, and accessory compatibility for different departments.
Hospitals should ensure the equipment meets CE, FDA, and ISO standards, along with local medical device registration to guarantee compliance and patient safety.
Standard packages include biopsy forceps, snares, injection needles, hemostasis clips, cleaning brushes, and optional stent placement kits.
XBX provides certified devices with HD imaging, customizable OEM/ODM solutions, comprehensive after-sales support, and competitive global procurement options tailored for hospitals.
Upper endoscopy helps doctors look inside the esophagus, stomach, and duodenum to find causes of heartburn, bleeding, ulcers, or unexplained stomach pain.
Most patients only feel mild throat discomfort. Sedation is usually given, so the procedure is not painful and patients often do not remember much of it.
The actual procedure usually lasts 15 to 30 minutes, although patients spend a few hours in the clinic including preparation and recovery time.
Most patients rest until the sedative wears off, may feel slight throat irritation, and can return to normal activities by the next day. Doctors will explain findings and next steps.
Copyright © 2025.Geekvalue All rights reserved.Technical Support:TiaoQingCMS