Table of Contents
A medical endoscope is a specialized instrument used to visually examine internal organs and cavities through minimally invasive procedures, providing real-time imagery for diagnosis and procedural guidance. These devices support clinical workflows in hospitals and surgical centers by enabling detailed internal assessment with reduced patient recovery time and improved procedural efficiency.
The medical term for scope denotes an instrument designed to provide internal visualization of body cavities, channels, or organs. In clinical practice this term covers a family of devices adapted for specific anatomical regions and clinical needs. Procurement teams and clinical leads use precise terminology to match equipment to departmental requirements, ensuring the right medical scope is chosen for each application.
Gastroscope refers to devices for upper digestive tract inspection, allowing targeted visualization and tissue sampling
Bronchoscope is used for airway and lung assessment, supporting diagnostic sampling and therapeutic interventions
Cystoscope enables visualization of the bladder and lower urinary tract for diagnosis and minor procedures
Arthroscope is designed for joint inspection and minimally invasive repairs
Consistent naming reduces procurement errors and ensures compatibility with existing systems
Clear definitions help define training curricula and technical maintenance requirements
Uniform terminology supports accurate clinical documentation and device tracking
Endoscopy is the clinical process of using specialized endoscopy tools to view, diagnose, and sometimes treat conditions inside the body without large incisions. In hospital workflows endoscopy supports diagnostics, interventional procedures, and postoperative evaluation. Devices range from simple optical scopes to advanced digital systems that integrate imaging, insufflation, irrigation, and working channels for instruments.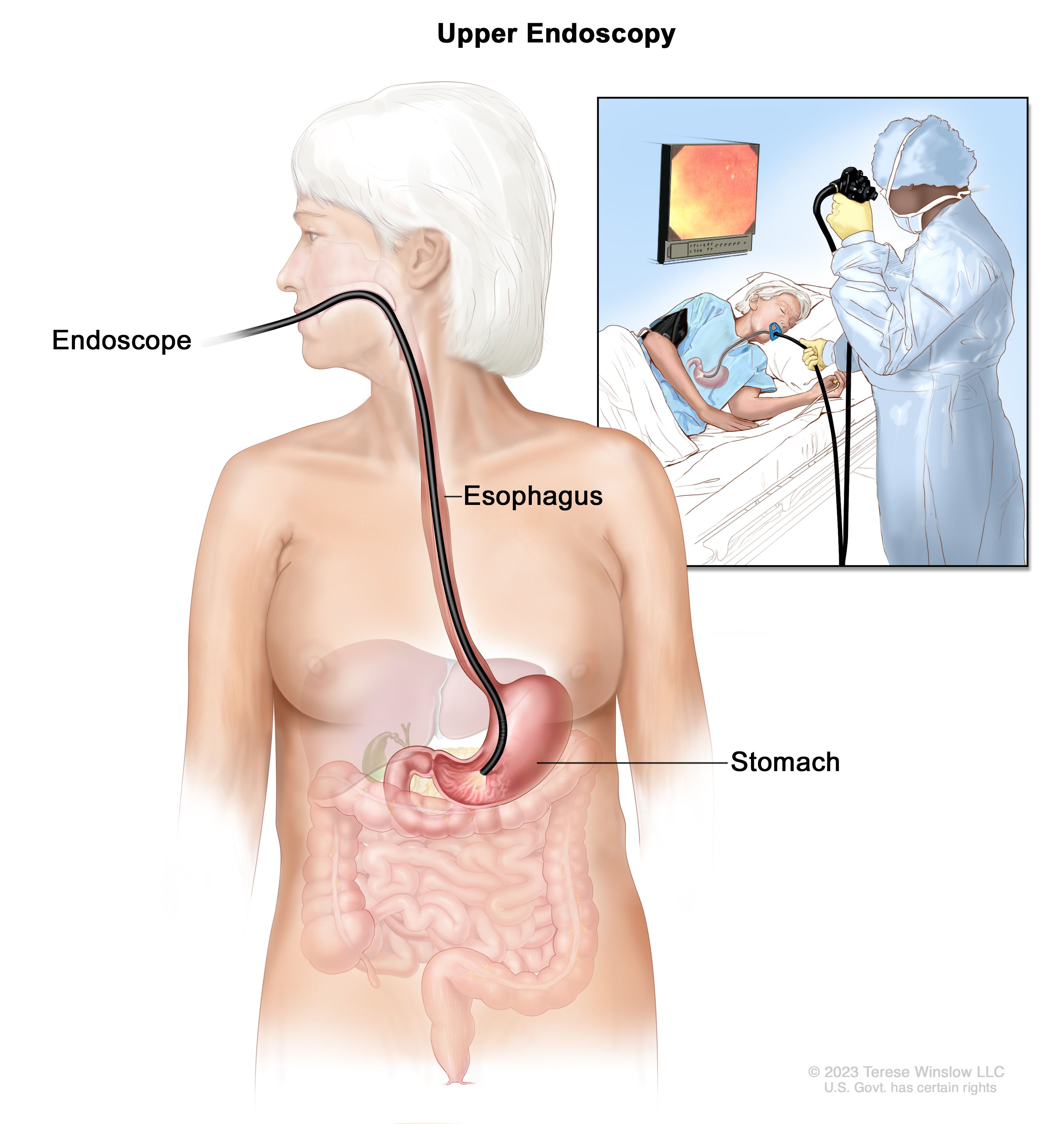
Diagnostic inspection of mucosal surfaces and internal anatomy
Biopsy sampling for pathology analysis
Therapeutic interventions such as polyp removal or foreign body extraction
Intraoperative visualization to guide minimally invasive surgery
Scheduling and room turnover depend on efficient reprocessing of endoscopy tools
Interdepartmental coordination improves utilization rates and reduces procedure delays
Integration with imaging recording systems supports quality assurance and teaching
An endoscope is the physical device used during endoscopy procedures. It typically includes an insertion tube, a control section, an illumination source, and an imaging system. Modern endoscopes use either fiber optics or digital sensors to capture images and relay them to a monitor in real time. Accessory channels permit passage of instruments, suction, or irrigation, enabling both diagnostic and therapeutic functions.
Insertion tube adapted for flexible or rigid navigation depending on clinical need
Control section for angulation and manipulation at the proximal end
Illumination system providing consistent light to ensure clear visualization
Imaging sensor or optical relay transmitting high resolution images to displays
Flexible endoscopes designed to navigate tortuous anatomy such as the colon or airways
Rigid endoscopes used when stability and precise instrument control are critical
Single use and reusable formats to balance infection control and cost effectiveness
Endoscopy tools enable clinicians to make timely, accurate assessments and carry out interventions with less trauma than open surgery. High quality imaging and reliable instrument channels reduce procedural time and support precise therapeutic maneuvers. Selection of appropriate endoscopy tools contributes directly to diagnostic confidence and operational efficiency in hospital practice.
Resolution and color fidelity influence lesion detection rates
Frame rate stability supports smooth real-time navigation during interventions
Recording capability aids multidisciplinary review and education
Ergonomic controls reduce operator fatigue during lengthy procedures
Well designed accessory channels simplify instrument exchanges
Reliable illumination and lens protection minimize interruptions during use
Different medical scopes are tailored to specific clinical domains and anatomical targets. Choosing the correct type of scope for a department ensures optimized image access and procedural efficiency. Procurement teams evaluate scope classes according to clinical procedures performed, expected case volume, and compatibility with existing infrastructure.
Gastroscopes for esophagus, stomach, and duodenum diagnostics and interventions
Colonoscopes for colorectal evaluation and screening programs
Bronchoscopes for airway inspection, sampling, and therapeutic airway management
Cystoscopes for urology diagnostics and minor endourologic procedures
Laparoscopes for abdominal and pelvic minimally invasive surgery
Arthroscopes for joint inspection and repair in orthopedics
Procedure specific features such as channel diameter and bending radius matter
Pediatric and bariatric use require specialized device sizing
Compatibility with monitoring and recording equipment ensures clinical integration
Procurement of endoscopy systems involves evaluating clinical requirements, total cost of ownership, compatibility with reprocessing workflows, and vendor support. Hospital purchasers consider device durability, upgrade paths, training programs, and service level agreements when selecting equipment for departments that rely on endoscopy tools.
Device reliability and expected lifecycle to estimate ongoing costs
Ease of cleaning and compatibility with existing reprocessing systems
Availability of spare parts and technical support networks
Training offerings to accelerate clinician competency and safe use
Balance between upfront capital cost and long term maintenance expenses
Evaluation of single use versus reusable devices based on infection control and throughput
Integration costs for image management and documentation systems
Consistent maintenance and validated sterilization protocols are essential to safeguard patient safety and extend the service life of medical scopes. Hospitals implement standard operating procedures that include precleaning, manual cleaning, high level disinfection or sterilization, and secure storage to minimize damage and contamination risk.
Initial point of use cleaning to remove gross debris
Manual cleaning with compatible detergents and brushes for channels
Automated high level disinfection or sterilization when appropriate
Routine inspection and leak testing prior to reuse
Designated reprocessing teams promote consistency and throughput
Documentation and traceability aid regulatory compliance and recall readiness
Preventive maintenance schedules reduce unexpected downtime
Effective use of a medical scope requires both procedural skill and familiarity with device mechanics. Hospitals invest in structured education programs that combine hands on practice, simulation training, and supervised clinical experience to ensure clinicians and support staff operate equipment safely and efficiently.
Simulation based modules for technical skills and complication management
Workshops led by clinical educators and device specialists
Proctoring during early clinical cases to reinforce best practices
Continuing education to keep teams updated on new tools and techniques
Reduced procedural complications and improved patient throughput
Faster onboarding for new clinicians and technicians
Better utilization of device capabilities through familiarization
Technological advances such as enhanced imaging, artificial intelligence assistance, capsule endoscopy, and robotic integration are expanding the capabilities of endoscopy tools. These innovations provide new diagnostic options and support more precise therapeutic interventions, while evolving hospital requirements for data integration and clinical workflow design.
AI driven image analysis to assist lesion detection and classification
Capsule devices offering non invasive visualization of the small intestine
Disposable scopes that streamline infection control procedures
Robotic and navigation aids improving precision in complex interventions
Investment in adaptable platforms supports future upgrades
Interoperability with electronic medical records and image archives is important
Staff development plans should include emerging technology training
Selecting a supplier that aligns with clinical goals and operational needs reduces risk and supports consistent performance. Buyers evaluate supplier capabilities in device customization, warranty and service coverage, training programs, and compliance with applicable medical device standards.
Range of products and options for customization to clinical protocols
Depth of technical support and responsiveness for repair and maintenance
Quality management systems and regulatory compliance documentation
References from other healthcare institutions with similar needs
Coordinated upgrade paths and predictable maintenance planning
Integrated training and performance reviews to maintain clinical standards
Collaborative planning for new service lines or specialty programs
A medical endoscope is a central instrument in modern diagnostic and interventional care. Understanding the medical term for scope, the range of endoscopy tools, procurement criteria, and maintenance and training practices helps hospitals and distributors make informed decisions that align with clinical demands and operational goals. Careful selection of devices and suppliers supports high quality patient care and efficient departmental performance. XBX
A medical endoscope is a specialized instrument that provides minimally invasive internal visualization for diagnosis and treatment. Hospitals use it for procedures such as gastroscopy, bronchoscopy, cystoscopy, and arthroscopy.
Common types include gastroscopes, bronchoscopes, cystoscopes, arthroscopes, colonoscopes, and laparoscopes, each designed for specific anatomical regions and procedures.
Hospitals evaluate clinical needs, procedure volumes, device compatibility with existing workflows, image quality, and ease of reprocessing to select the most appropriate endoscope.
Modern endoscopes consist of a flexible or rigid insertion tube, control section, illumination system, imaging sensor, and accessory channels for instruments and irrigation.
Choosing suppliers with strong technical support, customization options, compliance certifications, and training services helps hospitals maintain equipment performance and clinical standards.
Considerations include infection control policies, procedure volume, cost of reprocessing, device durability, and budget constraints.
Copyright © 2025.Geekvalue All rights reserved.Technical Support:TiaoQingCMS