Оглавление
Стоимость гастроскопии в 2025 году варьируется от 150 до 800 долларов США за процедуру для пациентов и от 5000 до более чем 40 000 долларов США на закупку оборудования в зависимости от региона, уровня больницы, бренда и модели закупки. Самые высокие цены зафиксированы в развитых странах, таких как США и Западная Европа, а самые низкие — в Китае и Индии, что делает закупки OEM/ODM привлекательным вариантом для покупателей.
Цена на гастроскопию в 2025 году отражает как клинические расходы пациентов, так и расходы медицинских учреждений на закупки. Во всем мире цены на процедуры варьируются в зависимости от уровня больницы, наличия медицинской страховки и условий местного рынка, в то время как цены на оборудование зависят от технологий, репутации бренда и масштаба закупок. Эта двойная структура означает, что больницы должны найти баланс между доступностью для пациентов и долгосрочными инвестициями в передовые эндоскопические системы.
Обычно пациенты платят за процедуру от 150 до 800 долларов США.
Больницы могут инвестировать от 5000 до 40 000 долларов США и более в закупку оборудования.
Системы страхования существенно влияют на доступность.
Между развитыми и развивающимися странами существуют рыночные различия.
Факторы, влияющие на стоимость гастроскопии в 2025 году, многогранны: от статуса больницы и региональных различий в системе здравоохранения до марок оборудования, уровня технологий и моделей закупок. Ценовая стратегия больницы часто зависит от её репутации, инфраструктуры и демографического состава пациентов, в то время как менеджеры по закупкам оценивают структуру затрат с учётом контрактов на техническое обслуживание, одноразовых принадлежностей и долгосрочной сервисной поддержки.
В ведущих больницах развитых стран цены на гастроскопию выше благодаря развитой инфраструктуре, квалифицированным специалистам и высококачественному послеоперационному уходу. В то же время, в муниципальных больницах или сельских клиниках процедуры часто обходятся дешевле, хотя иногда и с использованием менее современного оборудования.
Международные бренды, такие как Olympus, Fujifilm и Pentax, часто задают высокие стандарты качества на рынке гастроскопического оборудования. Китайские и корейские производители, напротив, ведут агрессивную ценовую конкуренцию, предлагая устройства на 20–40% дешевле, но при этом соответствующие международным сертификатам качества. Выбор между этими вариантами влияет как на стоимость закупки, так и на стоимость услуг для пациентов.
Когда больницы или дистрибьюторы закупают гастроскопическое оборудование у поставщиков OEM/ODM, они получают скидки при покупке большого количества оборудования и возможность адаптировать его к индивидуальным требованиям. Индивидуальное брендирование и специализированные конфигурации могут влиять на стоимость, но цена за единицу при крупных заказах часто значительно ниже, чем при покупке поштучно.
Гастроскопы высокой чёткости (HD) и 4K, передовые видеопроцессоры и инструменты обнаружения на базе искусственного интеллекта способствуют росту цен. Оптоволоконные эндоскопы начального уровня всё ещё доступны по более низким ценам, но в отрасли наблюдается тенденция перехода к видеосистемам, обеспечивающим более чёткое изображение и электронное документирование.
Уровень больницы и сложность обслуживания.
Репутация бренда и страна происхождения.
Возможности OEM/ODM-индивидуализации.
Технологии обработки изображений (HD, 4K, AI).
Долгосрочное обслуживание и расходные материалы.
Региональные различия являются одним из важнейших факторов, определяющих стоимость гастроскопии, отражая различия в экономическом потенциале, политике здравоохранения и уровне проникновения технологий. В то время как в развитых странах стоимость оборудования и процедур выше, развивающиеся регионы предлагают более доступные варианты, но могут сталкиваться с ограничениями в сетях обслуживания и требованиях к разрешительным документам. Это делает глобальный бенчмаркинг крайне важным для больниц и специалистов по закупкам.
В США и Западной Европе стоимость гастроскопии обычно составляет от 400 до 800 долларов США, в зависимости от того, включены ли анестезия и биопсия. Затраты на закупку оборудования остаются высокими, при этом стоимость премиальных систем превышает 35 000 долларов США за единицу. Строгие нормативные требования и политика возмещения расходов способствуют повышению цен.
В Китае и Индии стоимость гастроскопии одна из самых низких, зачастую от 100 до 300 долларов. Однако спрос на оборудование быстро растёт благодаря расширению сети больниц и государственным инвестициям в здравоохранение. Корея и Япония представляют собой среднюю ценовую зону с конкурентоспособными производителями и передовыми системами визуализации.
В этих регионах наблюдается более широкий диапазон цен. Частные больницы в странах Персидского залива могут соответствовать европейским ценам, в то время как многие клиники в Африке и Латинской Америке предлагают процедуры по цене менее 200 долларов. Проблемы с закупками, импортные пошлины и сбои в цепочке поставок часто приводят к завышению стоимости оборудования в этих регионах, несмотря на более низкую стоимость процедур.
| Область | Стоимость процедуры (долл. США) | Стоимость оборудования (долл. США) |
|---|---|---|
| Северная Америка | 400–800 | 25,000–40,000 |
| Западная Европа | 350–750 | 25,000–38,000 |
| Китай/Индия | 100–300 | 5,000–15,000 |
| Корея/Япония | 200–500 | 12,000–25,000 |
| Средний Восток | 250–600 | 20,000–35,000 |
| Африка / Латинская Америка | 100–250 | 8,000–20,000 |
Северная Америка/Европа: самые высокие цены, надежное страховое покрытие.
Китай/Индия: самые низкие затраты на процедуры, конкурентоспособное оборудование.
Ближний Восток: Разнообразие частных больниц, отражающих европейский уровень.
Африка/Латинская Америка: низкие процедурные сборы, но более высокие затраты на импорт.
Понимание разницы между стоимостью гастроскопии для медицинских учреждений и стоимостью, взимаемой с пациентов, крайне важно для точного финансового планирования. Больницы несут значительные первоначальные расходы на приобретение эндоскопических систем, в то время как пациенты оценивают доступность, основываясь на собственных расходах и страховом покрытии. Сочетание этих двух факторов формирует общую экосистему ценообразования в здравоохранении.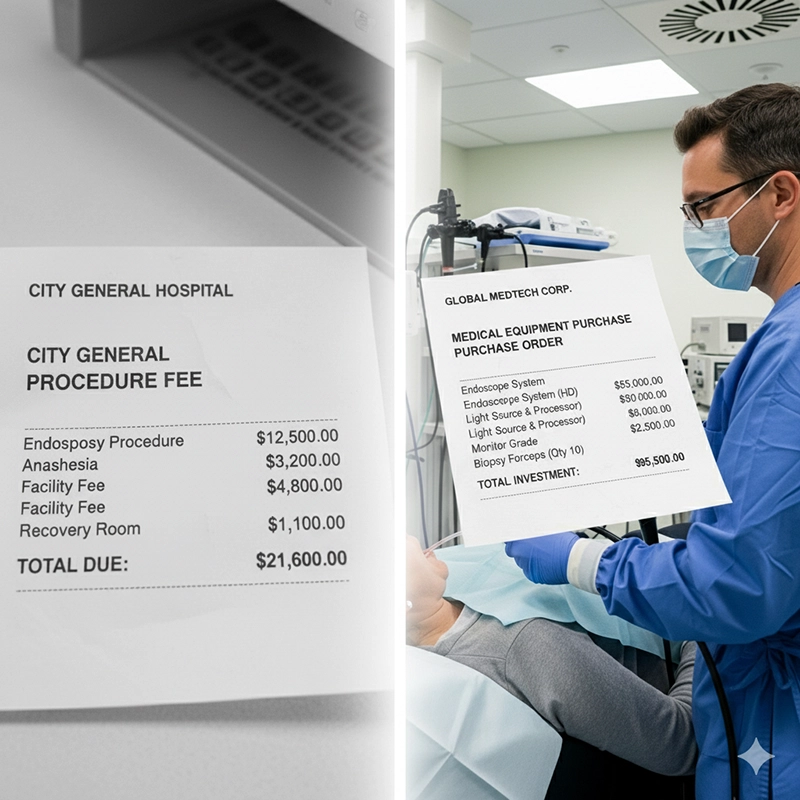
Больницам, инвестирующим в гастроскопическое оборудование, необходимо взвесить первоначальные затраты на его приобретение и долгосрочную выгоду. Премиальная система с передовыми технологиями визуализации может потребовать более высоких капитальных затрат, но может обеспечить лучшие результаты диагностики и доверие пациентов.
Стоимость гастроскопии для пациентов зависит от расходов на персонал, использования анестезии и лабораторных исследований. Даже при закупке оборудования со скидкой стоимость для пациентов может оставаться высокой в регионах со значительными накладными расходами в больницах.
Контракты на сервисное обслуживание, запасные части и одноразовые принадлежности, такие как биопсийные щипцы и чистящие щётки, увеличивают текущие расходы. Эти скрытые расходы часто составляют 10–15% от общей стоимости владения за весь срок службы.
Закупка оборудования: первоначальные инвестиции, которые часто являются основной статьей расходов.
Стоимость процедуры: зависит от численности персонала, анестезии и лабораторных работ.
Контракты на техническое обслуживание: охватывают обслуживание, калибровку и обновление программного обеспечения.
Расходные материалы: одноразовые щипцы, щетки для чистки и аксессуары.
Личное потребление и платёжеспособность существенно влияют на то, как больницы устанавливают цены на эндоскопические услуги и как отделы закупок планируют инвестиции. В регионах, где пациенты в основном платят из собственного кармана, учреждения часто снижают цены на услуги, что ограничивает бюджеты на закупку оборудования. И наоборот, развитые системы страхования позволяют больницам внедрять премиальные технологии, не беспокоясь о доступности услуг для пациентов.
В регионах, где пациентам приходится оплачивать значительную часть стоимости гастроскопии из собственного кармана, больницы часто корректируют ценовую политику в сторону снижения, чтобы сохранить доступность. Это напрямую влияет на решения о закупках, поскольку учреждения могут выбирать оборудование среднего класса вместо систем премиум-класса, чтобы сбалансировать доступность и устойчивость.
Страны с широким страховым покрытием, такие как Германия или Япония, позволяют больницам закупать более дорогие гастроскопические системы, поскольку возмещение расходов смягчает нагрузку на пациентов. В отличие от этого, рынки с высокой долей самооплаты, такие как Индия, вынуждают больницы поддерживать низкие цены на процедуры, что часто побуждает менеджеров по закупкам закупать оборудование у OEM/ODM-поставщиков по более низкой цене.
Общая потребительская способность населения создаёт обратную связь: более высокий уровень дохода позволяет больницам взимать более высокую плату за процедуру, что, в свою очередь, стимулирует инвестиции в современное оборудование. Напротив, более низкий уровень дохода ограничивает как объём услуг, так и покупательную способность больниц.
Более низкий доход домохозяйств заставляет больницы выбирать системы среднего уровня.
Рынки, ориентированные на страхование, способствуют внедрению премиальных технологий.
Доступность услуг для пациентов напрямую ограничивает потолок цен на процедуры.
Между уровнями доходов и бюджетами больниц существует сильная обратная связь.
Для больниц, дистрибьюторов и менеджеров по закупкам оценка вариантов OEM и заводского производства критически важна для управления долгосрочными расходами. Заводы предлагают более выгодные цены для оптовых партий и возможности кастомизации, а дистрибьюторы обеспечивают логистику и послепродажную поддержку. Баланс этих двух каналов имеет ключевое значение для достижения устойчивых стратегий закупок на рынке гастроскопии.
OEM- и ODM-заводы, особенно в Азии, поставляют гастроскопы, изготовленные по индивидуальному заказу, дистрибьюторам по всему миру. Эти решения снижают себестоимость единицы продукции и позволяют региональным дистрибьюторам выпускать продукцию под местными торговыми марками.
Больницы, заказывающие оптом, получают более низкие цены за единицу, что иногда позволяет сэкономить на 30–40% по сравнению с закупками поштучно. Дистрибьюторы, объединяющие спрос между несколькими больницами, также получают выгодные цены от производителя.
Прямые закупки у производителей гастроскопов снижают посреднические расходы. Однако дистрибьюторы обеспечивают послепродажное обслуживание и упрощают логистику, что оправдывает их более высокие цены на многих рынках.
OEM-заводы: более низкие цены за единицу при оптовых заказах.
Поставщики ODM: индивидуальный брендинг и индивидуальные конфигурации.
Дистрибьюторы: дополнительная сервисная поддержка, более высокие первоначальные затраты.
Прямые поставки с завода: сокращение числа посредников, повышение ответственности.
Перспективы ценообразования на эндоскопию отражают совокупное влияние демографических изменений, технологических инноваций и политики здравоохранения. Растущий спрос на ранний скрининг рака, наряду с государственными инвестициями в здравоохранение, будет способствовать росту стоимости процедур и закупок оборудования. Учреждения, планирующие свою деятельность на следующее десятилетие, должны быть готовы к более высоким первоначальным затратам, а также к потенциальному повышению эффективности благодаря новым технологиям.
Прогнозируется, что рынок гастроскопического оборудования будет расти среднегодовыми темпами на 6–8% в период с 2025 по 2030 год, что обусловлено старением населения, ростом программ скрининга рака и расширением доступа к здравоохранению в развивающихся странах (Statista, 2024).
Выявление поражений с помощью искусственного интеллекта, усовершенствованные видеопроцессоры и одноразовые эндоскопы меняют структуру цен на гастроскопию. Хотя инновации изначально увеличивают стоимость оборудования, в долгосрочной перспективе они могут снизить стоимость процедур за счёт повышения эффективности и сокращения числа повторных процедур.
Государственные программы, расширяющие охват скринингом, такие как инициативы Китая по профилактике рака или реформы цифрового здравоохранения в ЕС, помогают стабилизировать стоимость процедур и стимулируют инвестиции больниц в современное оборудование.
Расширение использования ИИ для раннего обнаружения поражений.
Растущий спрос на одноразовые эндоскопы для контроля инфекций.
Прогнозируемый среднегодовой темп роста рынка составит 6–8%.
Расширение программ скрининга по всему миру на основе проводимой политики.
При покупке гастроскопических систем менеджерам по закупкам необходимо учитывать широкий спектр критериев. Помимо первоначальной цены, от общей стоимости владения, гарантийного обслуживания и надежности поставщика зависят и долгосрочные преимущества инвестиций. Покупателям рекомендуется использовать структурированные процессы закупок, учитывающие как технические характеристики, так и долгосрочную экономическую целесообразность.
Покупатели должны проверять соответствие нормативным требованиям (например, CE, FDA) и оценивать историю надежности обслуживания. Помимо цены, важны прозрачность поставщика и сети поддержки.
Больницы не могут полагаться исключительно на самую низкую цену гастроскопии. Более дешёвое оборудование без сервисной поддержки может привести к простоям, снижению точности диагностики и скрытым расходам. Баланс заключается в выборе поставщиков, которые предлагают как доступную цену, так и надёжное послепродажное обслуживание.
Обеспечить совместимость с существующими эндоскопическими системами.
Ознакомьтесь с условиями гарантии и обязательствами по техническому обслуживанию.
Оцените общую стоимость владения за 5–10 лет.
Учитывайте долгосрочную доступность запасных частей и расходных материалов.
Сравните общую стоимость владения, а не только цену покупки.
Обеспечить соответствие поставщика сертификатам CE/FDA.
Уделяйте первостепенное внимание послепродажному обслуживанию и доступности запасных частей.
Баланс требований к качеству и долгосрочной доступности.
Цена на гастроскопию в 2025 году остаётся сложной формулой, определяемой глобальной экономикой, потребительским спросом, системами страхования и технологическим прогрессом. Для пациентов доступность оборудования диктует доступ к ранней диагностике и профилактическим медицинским услугам. Для больниц и менеджеров по закупкам решения основаны на балансе первоначальных затрат на оборудование с моделями устойчивого ценообразования процедур. Независимо от того, закупаете ли вы оборудование у премиальных международных брендов или у экономичных OEM/ODM-производителей, основополагающий принцип остаётся неизменным: при выборе закупок следует учитывать как экономическую целесообразность, так и клиническое совершенство.
Средняя заводская цена на оптовые заказы составляет от 5000 до 15 000 долларов США за единицу, при заказе свыше 20 единиц предоставляются значительные скидки.
Да, доступна возможность настройки OEM/ODM, включая брендинг, технические характеристики и упаковку, соответствующие требованиям больницы или дистрибьютора.
Стоимость премиальных международных брендов может составлять от 25 000 до 40 000 долларов США за единицу, в то время как заводские гастроскопы OEM/ODM могут быть на 30–40 % более экономичными.
Факторы включают объем заказа, техническую конфигурацию (HD, 4K, AI), послепродажное обслуживание и региональные импортные пошлины.
Доставка стандартных моделей обычно занимает 4–6 недель, а заказных OEM/ODM-устройств — 8–12 недель.
Авторские права © 2025.Geekvalue. Все права защищены.Техническая поддержка: TiaoQingCMS