विषयसूची
घुटने की आर्थ्रोस्कोपी एक न्यूनतम आक्रामक प्रक्रिया है जिसका उपयोग एक छोटे से चीरे और विशेष एंडोस्कोपिक उपकरणों के माध्यम से विभिन्न जोड़ों की स्थितियों का निदान और उपचार करने के लिए किया जाता है। अस्पतालों में, यह सर्जनों को घुटने की आंतरिक संरचनाओं को सटीकता से देखने, उनका आकलन करने और उनका प्रबंधन करने की अनुमति देता है, जिससे शल्य चिकित्सा संबंधी आघात कम होता है और कार्यात्मक सुधार तेज़ी से संभव होता है। सटीक निदान और लक्षित उपचार के लिए यह तकनीक आर्थोपेडिक देखभाल का एक महत्वपूर्ण हिस्सा बन गई है।

एकआर्थ्रोस्कोपीफैक्ट्री उच्च-गुणवत्ता वाले आर्थ्रोस्कोपिक उपकरणों के लिए स्रोत बिंदु के रूप में कार्य करती है जो सटीक अस्पताल प्रक्रियाओं का समर्थन करते हैं। ये सुविधाएँ ऐसे उपकरणों का डिज़ाइन और उत्पादन करती हैं जो सुरक्षा, स्थायित्व और स्पष्टता के लिए सख्त चिकित्सा मानकों को पूरा करते हैं। B2B खरीद टीमों के लिए, एक विश्वसनीय विनिर्माण स्रोत के साथ साझेदारी उन्नत ऑप्टिकल सिस्टम, एर्गोनॉमिक डिज़ाइन और विभिन्न सर्जिकल सेटिंग्स के अनुकूल अनुकूलनीय उपकरणों तक पहुँच सुनिश्चित करती है।
आर्थोस्कोपी निर्माता अत्याधुनिक शल्य चिकित्सा उपकरणों के विकास में अभिन्न अंग हैं। वे लेंस की गुणवत्ता, प्रकाश व्यवस्था और उपकरणों की गतिशीलता में नवाचार पर ध्यान केंद्रित करते हैं, जिससे सर्जन संयुक्त स्थान के अंदर कुशलतापूर्वक काम कर पाते हैं। ये निर्माता घुटने की विभिन्न स्थितियों, लिगामेंट की चोटों से लेकर कार्टिलेज की मरम्मत तक, के लिए अनुकूलित विभिन्न प्रकार के स्कोप और सहायक उपकरण भी प्रदान करते हैं, जिससे यह सुनिश्चित होता है कि अस्पताल एक ही मूल तकनीक से कई प्रकार की प्रक्रियाएँ कर सकें।
स्पष्ट अंतःक्रियात्मक छवियों के लिए उच्च-परिभाषा विज़ुअलाइज़ेशन प्रणालियाँ
ऊतक के पास गर्मी को कम करने के लिए कॉम्पैक्ट प्रकाश स्रोत
इष्टतम संयुक्त विस्तार और मलबे की निकासी के लिए द्रव प्रबंधन प्रणालियाँ
नसबंदी और रखरखाव को सरल बनाने के लिए मॉड्यूलर डिज़ाइन
एकआर्थोस्कोपी आपूर्तिकर्तानिर्माताओं और स्वास्थ्य सेवा प्रदाताओं के बीच की खाई को पाटता है। अस्पताल अक्सर समय पर डिलीवरी, उपकरण प्रशिक्षण और बिक्री के बाद तकनीकी सहायता के लिए आपूर्तिकर्ताओं पर निर्भर रहते हैं। बड़े पैमाने पर खरीद के लिए, एक स्थापित आपूर्तिकर्ता उत्पाद की गुणवत्ता में स्थिरता प्रदान कर सकता है, अस्पताल के प्रोटोकॉल का अनुपालन सुनिश्चित कर सकता है, और विशिष्ट प्रक्रियात्मक वर्कफ़्लो के अनुरूप अनुकूलन प्रदान कर सकता है।
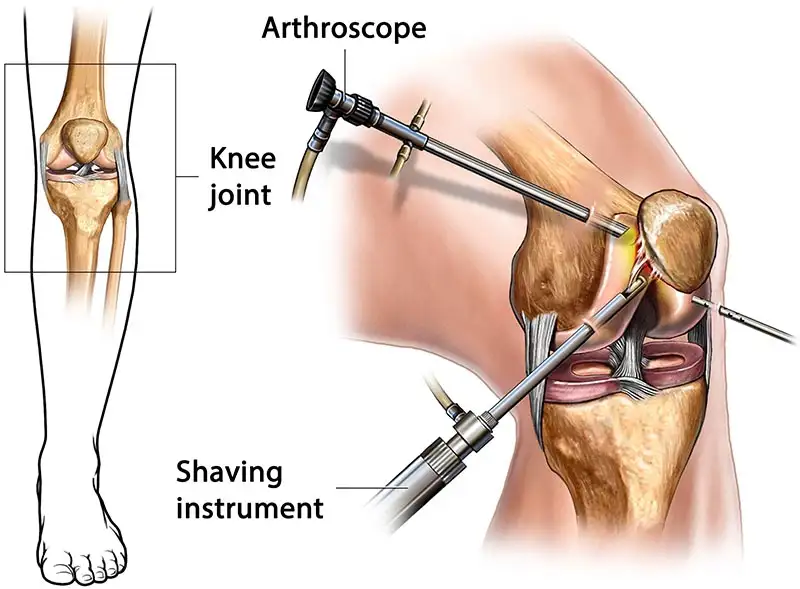
घुटने की आर्थ्रोस्कोपी में घुटने के जोड़ में एक छोटा कैमरा, जिसे आर्थ्रोस्कोप कहा जाता है, डालकर उपास्थि, स्नायुबंधन और आसपास के ऊतकों की जाँच की जाती है। यह विधि खुली सर्जरी की तुलना में स्वस्थ ऊतकों को होने वाले नुकसान को कम करती है। अस्पतालों में, यह उन मामलों में एक पसंदीदा विकल्प है जहाँ सटीक दृश्यता निदान संबंधी विश्वास और शल्य चिकित्सा की सटीकता में सुधार कर सकती है।
मेनिस्कल आँसू
लिगामेंट की चोटें जैसे ACL या PCL क्षति
उपास्थि का घिसना या घाव
सिनोवाइटिस के लिए ऊतक निष्कासन की आवश्यकता होती है
जोड़ में ढीली वस्तुएं
अस्पताल में, घुटने की आर्थोस्कोपिक सर्जरी मरीज़ की तैयारी और सटीक चीरा लगाने से शुरू होती है। आर्थोस्कोप वास्तविक समय की छवियों को मॉनिटर पर भेजता है, जिससे शल्य चिकित्सा दल जोड़ों के अंदर उपकरणों का उपयोग कर पाता है। ऊतक की छंटाई, मरम्मत या निष्कासन के लिए विशेष उपकरण द्वितीयक द्वारों के माध्यम से डाले जाते हैं। यह विधि आसपास के ऊतकों की अखंडता को बनाए रखते हुए नियंत्रित हस्तक्षेप का समर्थन करती है।

घुटने की आर्थोस्कोपिक सर्जरी से रिकवरी प्रक्रिया की जटिलता और मरीज की स्थिति पर निर्भर करती है। अस्पतालों के लिए, ऑपरेशन के बाद की देखभाल के प्रोटोकॉल में निर्देशित फिजियोथेरेपी, घाव की निगरानी और प्रगतिशील गतिशीलता कार्यक्रम शामिल हैं। अस्पताल श्रृंखलाओं जैसे B2B खरीद ग्राहक अक्सर आर्थोस्कोपिक रिकवरी योजनाओं के अनुकूल पुनर्वास उपकरणों में निवेश करते हैं, जिससे यह सुनिश्चित होता है कि मरीज़ कुशलतापूर्वक अपनी कार्यक्षमता वापस पा सकें।

सर्जिकल जटिलता और अवधि
रोगी के शल्यक्रिया-पूर्व संयुक्त स्वास्थ्य
फिजियोथेरेपी कार्यक्रम का पालन
अस्पताल-आधारित पुनर्वास संसाधनों की उपलब्धताअस्पताल के संदर्भ में घुटने की आर्थ्रोस्कोपी से ठीक होने में लगने वाला समय
एक नियंत्रित अस्पताल के वातावरण में, घुटने की आर्थ्रोस्कोपी से ठीक होने का समय रोगी के आधारभूत स्वास्थ्य और की गई प्रक्रिया के प्रकार पर निर्भर करता है। हालाँकि कुछ रोगी कुछ ही दिनों में बुनियादी गतिशीलता प्राप्त कर सकते हैं, लेकिन पूर्ण कार्यात्मक सुधार में कई हफ़्तों से लेकर महीनों तक का समय लग सकता है। अस्पताल संरचित समय-सीमा का उपयोग करते हैं, धीरे-धीरे भार वहन करने वाली गतिविधियों को आगे बढ़ाते हैं और छुट्टी देने से पहले जोड़ों की स्थिरता सुनिश्चित करते हैं।
प्रारंभिक सूजन नियंत्रण और दर्द प्रबंधन
बुनियादी संयुक्त गतिशीलता की बहाली
क्रमिक सुदृढ़ीकरण व्यायाम
पर्यवेक्षण के तहत कार्यात्मक गतिविधियों पर लौटें
घुटने की सर्जरी के दौरान सटीकता बनाए रखने के लिए उच्च-गुणवत्ता वाले आर्थ्रोस्कोपी उपकरण आवश्यक हैं। उन्नत ऑप्टिकल सिस्टम सर्जनों को उपास्थि या स्नायुबंधन में सूक्ष्म क्षति की पहचान करने में सक्षम बनाते हैं, जबकि अच्छी तरह से डिज़ाइन किए गए उपकरण तंग जोड़ों में स्थिर संचालन प्रदान करते हैं। खरीद टीमों के लिए, आधुनिक आर्थ्रोस्कोपिक प्रणालियों में निवेश यह सुनिश्चित करता है कि शल्य चिकित्सा विभाग कई ऑपरेटिंग थिएटरों में एक समान परिणाम दे सकें।
अस्पतालों और उनके आर्थोस्कोपी उपकरण प्रदाताओं के बीच एक उत्पादक संबंध, उपकरणों की निरंतर उपलब्धता, नई तकनीकों के त्वरित अनुकूलन और कुशल रखरखाव कार्यक्रमों को बढ़ावा देता है। यह सहयोग यह भी सुनिश्चित करता है कि शल्य चिकित्सा टीमों को नवीनतम उपकरणों की विशेषताओं का प्रशिक्षण दिया जाए, जिससे प्रक्रियात्मक दक्षता और रोगी देखभाल की गुणवत्ता में सुधार हो।
वैश्विक अस्पताल नेटवर्क में, विभिन्न सुविधाओं में आर्थोस्कोपी उपकरणों के विनिर्देशों का मानकीकरण एकीकृत प्रशिक्षण और रखरखाव को बढ़ावा देता है। अंतर्राष्ट्रीय वितरकों के लिए, विविध बाज़ारों की सेवा के लिए कई नियामक मानकों को पूरा करने वाले उपकरणों की आपूर्ति महत्वपूर्ण है। यह अनुकूलनशीलता खरीद दक्षता को बढ़ाती है और विभिन्न क्षेत्रों में एकसमान रोगी देखभाल को बढ़ावा देती है।
घुटने की आर्थ्रोस्कोपी, अस्पताल में जोड़ों की समस्याओं का प्रभावी ढंग से समाधान करने के लिए न्यूनतम इनवेसिव पहुँच और उन्नत विज़ुअलाइज़ेशन का संयोजन करती है।आर्थोस्कोपी कारखानाआवश्यक उपकरणों के उत्पादन से लेकर आपूर्तिकर्ताओं और निर्माताओं के बीच सहयोग तक, आपूर्ति श्रृंखला का प्रत्येक चरण शल्य चिकित्सा की सटीकता और पुनर्प्राप्ति परिणामों को प्रभावित करता है। अस्पताल, वितरक और खरीद दल अपने शल्य चिकित्सा कार्यक्रमों में उच्च-गुणवत्ता वाली आर्थ्रोस्कोपी प्रणालियों को एकीकृत करके आर्थोपेडिक देखभाल को बेहतर बना सकते हैं। विश्वसनीय आर्थ्रोस्कोपी समाधानों के लिए, XBX पेशेवर स्वास्थ्य देखभाल आवश्यकताओं के अनुरूप उन्नत उपकरण प्रदान करता है।
घुटने की आर्थ्रोस्कोपी अब विशुद्ध रूप से निदानात्मक भूमिका से कहीं आगे बढ़ चुकी है। आधुनिक अस्पतालों में, यह एक बहुमुखी, न्यूनतम आक्रामक प्लेटफ़ॉर्म के रूप में कार्य करता है जो सटीक दृश्यीकरण, लक्षित हस्तक्षेप और डेटा-आधारित परिचालन-पूर्व देखभाल का समर्थन करता है। यह खंड नवाचारों, अस्पताल एकीकरण रणनीतियों और कार्यक्रम-स्तरीय विचारों की समीक्षा करता है जो सुरक्षा, दक्षता और मूल्य को बनाए रखते हुए घुटने की आर्थ्रोस्कोपी के प्रभाव का विस्तार करते हैं।
प्रारंभिक घुटने की आर्थ्रोस्कोपी मुख्यतः पुष्टिकारक थी; आज यह निश्चित रूप से चिकित्सीय है। छोटे पोर्टल्स के माध्यम से, सर्जन मेनिस्कल टियर की मरम्मत करते हैं, फ़ोकल कॉन्ड्रल घावों का उपचार करते हैं, स्नायुबंधन का पुनर्निर्माण करते हैं, और न्यूनतम कोमल ऊतकों को नुकसान पहुँचाए बिना ढीले पिंडों को निकालते हैं। अस्पतालों के लिए, इस विकास के लिए एक पारिस्थितिकी तंत्र मानसिकता की आवश्यकता होती है: कैमरे, प्रकाश स्रोत, शेवर, द्रव पंप, विशेष उपकरण, और प्रमाणित पुनर्प्रसंस्करण। ये तत्व घुटने की आर्थ्रोस्कोपी को रोगी के रहने की अवधि को कम करने, जटिलताओं की दर को कम करने और कार्यात्मक पुनर्प्राप्ति में तेजी लाने में सक्षम बनाते हैं।
चिकित्सीय दायरा: मेनिस्कल मरम्मत, कोंड्रोप्लास्टी, माइक्रोफ्रैक्चर, ओस्टियोकॉन्ड्रल ग्राफ्टिंग, लिगामेंट पुनर्निर्माण।
प्रणाली दृष्टिकोण: इमेजिंग टावर, एर्गोनॉमिक रूप से अनुकूलित हस्त उपकरण, और मानकीकृत ट्रे विन्यास।
परिचालन उद्देश्य: सावधानीपूर्वक नियंत्रित कार्यप्रवाह के साथ टीमों और मामलों में पुनरुत्पादनीय परिणाम।
हाई-डेफिनिशन और 4K प्लेटफ़ॉर्म ने इंट्रा-आर्टिकुलर विज़ुअलाइज़ेशन को पूरी तरह बदल दिया है। अब सर्जन माइक्रोफ़िसर्स, कार्टिलेज के शुरुआती नरम होने और सिनोवियल पैथोलॉजी में ज़्यादा आत्मविश्वास से पहचान कर सकते हैं। बेहतर रंग सटीकता और कंट्रास्ट, निर्णय लेने के लिए ज़रूरी ऊतक संकेतों को सुरक्षित रखते हैं। चुनिंदा सिस्टम त्रि-आयामी विज़ुअलाइज़ेशन या संवर्धित ओवरले जोड़ते हैं जो प्रीऑपरेटिव इमेजिंग से प्राप्त स्थलों को सीधे आर्थ्रोस्कोपिक क्षेत्र पर मैप करते हैं, जिससे घुटने की आर्थ्रोस्कोपी के दौरान अभिविन्यास में सुधार होता है।
कम प्रकाश वाले संयुक्त स्थानों के लिए उच्च सिग्नल-टू-शोर इमेजिंग।
वास्तविक रंग संतुलन जो उपास्थि और मेनिस्कस संकेतों को संरक्षित करता है।
एमआरआई-व्युत्पन्न शरीर रचना को एकीकृत करने वाला वैकल्पिक एआर मार्गदर्शन।
आधुनिक शेवर, बर्स और रेडियोफ्रीक्वेंसी (आरएफ) प्रोब सटीकता और तापीय सुरक्षा को प्राथमिकता देते हैं। शेवर में परिवर्तनशील सक्शन नियंत्रण मलबे को सीमित करता है और दृश्यता को सुरक्षित रखता है। आरएफ उपकरण न्यूनतम संपार्श्विक ताप के साथ नियंत्रित एब्लेशन और हेमोस्टेसिस प्रदान करते हैं। हाथ के उपकरण एर्गोनॉमिक ग्रिप और आर्टिकुलेटिंग टिप्स पर ज़ोर देते हैं ताकि सर्जन की थकान को कम करते हुए पश्च भागों तक पहुँचा जा सके। द्रव प्रबंधन पंप अंतर्वाह/बहिर्वाह दाब की निगरानी करते हैं, कोमल ऊतकों की रक्षा करते हैं और घुटने की आर्थ्रोस्कोपी के दौरान बहिर्वाह को सीमित करते हैं।
त्वरित-कनेक्ट कपलिंग और मॉड्यूलर हैंडपीस उपकरण विनिमय को सुव्यवस्थित करते हैं।
दबाव-नियंत्रित पंप सूजन को कम करते हैं और एक स्पष्ट क्षेत्र बनाए रखते हैं।
डिस्पोजेबल ट्यूबिंग सेट और फिल्टर संक्रमण नियंत्रण नीतियों का समर्थन करते हैं।
आर्थोस्कोपी में यांत्रिक मरम्मत को जैविक वृद्धि के साथ जोड़ा जा रहा है। प्लेटलेट-समृद्ध प्लाज्मा (पीआरपी), अस्थि मज्जा एस्पिरेट सांद्र (बीएमएसी), और स्कैफोल्ड-आधारित तकनीकों का उद्देश्य उपास्थि (कॉन्ड्रल) की चिकित्सा को बेहतर बनाना है। जैविक पदार्थों के साथ संयुक्त माइक्रोफ्रैक्चर, भराव की गुणवत्ता और स्थायित्व में सुधार लाने का प्रयास करता है। ऐसे तरीकों पर विचार करने वाले अस्पताल क्षेत्रीय नियमों के अनुरूप सहायक उपकरणों (सेंट्रीफ्यूज, सेल प्रोसेसर), कर्मचारियों के प्रशिक्षण और दस्तावेज़ीकरण की योजना बनाते हैं - जैविक रूप से उन्नत घुटने की आर्थोस्कोपी के लिए एक सुसंगत, साक्ष्य-आधारित ढाँचा तैयार करते हैं।
ऑपरेटिंग रूम कनेक्टेड वातावरण में बदल रहे हैं। आर्थोस्कोपी टावर ऑडिट, शिक्षा और अनुसंधान के लिए वीडियो को कैप्चर, टैग और इलेक्ट्रॉनिक स्वास्थ्य रिकॉर्ड में निर्यात करते हैं। एआई-सहायता प्राप्त एनालिटिक्स वास्तविक समय में मेनिस्कल टियर या कार्टिलेज दोषों को चिह्नित करने के लिए उभर रहे हैं, जिससे अंतःक्रियात्मक गुणवत्ता में सुधार होता है। सुरक्षित नेटवर्क पर टेली-मेंटरिंग विशेषज्ञों को जटिल घुटने की आर्थोस्कोपी के मामलों का दूर से मार्गदर्शन करने की अनुमति देता है, जिससे अस्पताल प्रणाली में विशेषज्ञता का विस्तार होता है।
शिक्षण और गुणवत्ता आश्वासन के लिए परिणाम-लिंक्ड मेटाडेटा के साथ केस रिकॉर्डिंग।
पूर्वानुमानात्मक मॉडलिंग के लिए वीडियो विश्लेषण अनुसंधान पाइपलाइनें।
मानक-आधारित एकीकरण जो गोपनीयता और सुरक्षा का सम्मान करते हैं।
प्रशासक केवल पूँजी मूल्य का ही नहीं, बल्कि कुल मूल्य का भी मूल्यांकन करते हैं। हालाँकि टावर, कैमरे और पंप बड़े निवेश हैं, लेकिन डाउनस्ट्रीम दक्षताएँ—कम समय तक रुकना, कम बार दोबारा भर्ती होना, और काम पर जल्दी वापसी—लागत की भरपाई कर सकती हैं। अनुबंधों में उपभोग्य सामग्रियों (शेवर ब्लेड, आरएफ प्रोब, ट्यूबिंग), प्रशिक्षण और सेवा कवरेज का ध्यान रखा जाना चाहिए। रणनीतिक साझेदारियाँ खरीद को शिक्षा और अपटाइम गारंटी के साथ जोड़ती हैं, जिससे घुटने की आर्थ्रोस्कोपी की लागत स्थिर रहती है और गुणवत्ता की रक्षा होती है।
पूंजी + उपभोग्य वस्तुएं + सेवा को एकल कार्यक्रम लागत के रूप में विश्लेषण करें।
मात्रा-आधारित मूल्य निर्धारण और बहु-वर्षीय सेवा अनुबंधों का अनुसरण करें।
बेंचमार्क केस अवधि, टर्नओवर समय, और प्रथम-पास उपज।
घुटने की आर्थ्रोस्कोपी रुमेटोलॉजी (सिनोवियल बायोप्सी), ऑन्कोलॉजी (इंट्रा-आर्टिकुलर घावों की लक्षित बायोप्सी), और स्पोर्ट्स मेडिसिन (व्यापक देखभाल मार्ग) के साथ जुड़ी हुई है। साझा उपकरण पूल और सुसंगत नसबंदी नीतियाँ उपयोग और निवेश पर प्रतिफल को बढ़ाती हैं। बहु-विषयक क्लीनिक प्राथमिकता निर्धारण और पुनर्वास को सुव्यवस्थित करते हैं, जिससे यह सुनिश्चित होता है कि मरीज़ निदान से घुटने की आर्थ्रोस्कोपी और उसके बाद अनुकूलित चिकित्सा तक कुशलतापूर्वक संक्रमण कर सकें।
निपुणता के लिए त्रिभुजाकार कौशल और स्थानिक तर्क की आवश्यकता होती है। सिमुलेशन लैब—बॉक्स ट्रेनर, बेंचटॉप मॉडल और वीआर प्लेटफ़ॉर्म—प्रशिक्षुओं को पोर्टल प्लेसमेंट, मेनिस्कल ट्रिमिंग और लूज़-बॉडी रिट्रीवल का सुरक्षित अभ्यास करने देते हैं। वस्तुनिष्ठ मापदंड (समय, दक्षता, चिकित्सकजनित संपर्क) प्रगति का आकलन करते हैं। जिन अस्पतालों में पाठ्यक्रम में सिमुलेशन शामिल है, वहाँ ऑपरेशन के दौरान कम त्रुटियाँ और तेज़ सीखने की प्रक्रिया होती है, जिससे घुटने की आर्थ्रोस्कोपी में कार्यक्रम की निरंतरता बढ़ती है।
कौशल प्रगति: ड्राई-लैब → वी.आर. → कैडेवरिक → पर्यवेक्षित ओ.आर.
डेटा-संचालित फीडबैक योग्यता के लक्ष्यों को गति प्रदान करता है।
संरक्षित अभ्यास समय से आत्मविश्वास और रोगी सुरक्षा में सुधार होता है।
उन्नत आर्थ्रोस्कोपी तक पहुँच दुनिया भर में अलग-अलग है। उच्च आय वाले केंद्र 4K टावर और बायोलॉजिक एडजंक्ट लगाते हैं; संसाधन-सीमित अस्पताल टिकाऊ आधार प्रणालियों और लक्षित उपभोग्य सामग्रियों के उपयोग पर निर्भर हो सकते हैं। दूर-शिक्षा, नवीनीकृत उपकरण और साझा सेवा नेटवर्क इस अंतराल को कम कर सकते हैं। टिकाऊ, चरणबद्ध अपनाने से अस्पतालों को स्थानीय विशेषज्ञता और विश्वसनीय आपूर्ति श्रृंखलाओं का निर्माण करते हुए घुटने की आर्थ्रोस्कोपी को सुरक्षित रूप से शुरू करने की अनुमति मिलती है।
साक्ष्य रोगी के चयन में मार्गदर्शन करते हैं। हालाँकि वृद्ध वयस्कों में अपक्षयी मेनिस्कल लक्षण गैर-शल्य चिकित्सा देखभाल से ठीक हो सकते हैं, तीव्र फटना, यांत्रिक लक्षण, स्नायुबंधन की चोट और फोकल उपास्थि विकृति अक्सर आर्थोस्कोपी से लाभान्वित होती है। अस्पताल अपेक्षाओं और परिणामों को संरेखित करते हुए संकेत प्रोटोकॉल और साझा निर्णय सहायता विकसित करते हैं। घुटने की आर्थोस्कोपी के बाद रोगी द्वारा रिपोर्ट किए गए परिणाम मापकों (PROMs) का लगातार संग्रह गुणवत्ता में सुधार और भुगतानकर्ता की सहभागिता को सूचित करता है।
संकेत एल्गोरिदम शल्य चिकित्सा संबंधी निर्णयों में परिवर्तनशीलता को कम करते हैं।
नियमित PROMs सर्जनों और साइटों के बीच बेंचमार्किंग को सक्षम बनाता है।
रजिस्ट्री की भागीदारी अनुसंधान और जवाबदेही को समर्थन देती है।
उपकरण की सुरक्षा प्रमाणित सफाई और स्टरलाइज़ेशन पर निर्भर करती है। स्वचालित एंडोस्कोप रीप्रोसेसर, निम्न-तापमान स्टरलाइज़ेशन और स्पष्ट रूप से चित्रित IFU के साथ संगतता, क्रॉस-संक्रमण के जोखिम को कम करती है। योग्यता-आधारित प्रशिक्षण, प्रक्रिया ऑडिट और ट्रेस करने योग्य लॉग, कस्टडी की एक सुरक्षित श्रृंखला बनाते हैं। एकल-उपयोग विज़ुअलाइज़ेशन विकल्प चुनिंदा मामलों में रसद को सरल बना सकते हैं, हालाँकि घुटने के आर्थ्रोस्कोपी कार्यक्रमों में लागत और पर्यावरणीय समझौतों की सावधानीपूर्वक समीक्षा की आवश्यकता होती है।
पूर्व-सफाई, रिसाव परीक्षण, सफाई, उच्च-स्तरीय कीटाणुशोधन/नसबंदी और भंडारण को मानकीकृत करें।
AER चक्रों और रसायन विज्ञान को उपकरण सामग्री सीमाओं के साथ संरेखित करें।
लेखापरीक्षा दस्तावेजीकरण: लॉट संख्या, चक्र आईडी, और रिलीज मानदंड।
मरीज़ कम से कम निशान, कम दर्द और जल्दी से काम पर लौटने को महत्व देते हैं। स्पष्ट पूर्व-संचालन शिक्षा—पोर्टल, एनेस्थीसिया विकल्प, यथार्थवादी समय-सीमा—विश्वास का निर्माण करती है। पोस्टऑपरेटिव योजनाएँ जो दर्द निवारक प्रबंधन, सूजन नियंत्रण और शीघ्र गति को जोड़ती हैं, चिंता को कम करती हैं और लक्ष्यों को शीघ्रता से प्राप्त करती हैं। सुलभ संचार माध्यम टीमों को चिंताओं का तुरंत समाधान करने में मदद करते हैं, जिससे घुटने की आर्थ्रोस्कोपी के बाद संतुष्टि में सुधार होता है।
ऑपरेशन-पूर्व शिक्षा: अपेक्षाएं, जोखिम और पुनर्वास मानचित्र।
ऑपरेशन के बाद की आवश्यक बातें: आर.आई.सी.ई., घाव की देखभाल, और लाल-झंडा लक्षण।
अनुवर्ती ताल: प्रारंभिक जांच, 6 से 12 सप्ताह तक कार्यात्मक समीक्षा।
ऑपरेटिंग रूम से काफ़ी कचरा निकलता है। कार्यक्रम पैकेजिंग को एकीकृत करके, जहाँ तक संभव हो पुनर्चक्रण योग्य सामग्री का चयन करके, और पर्यावरण-अनुकूल किटों के लिए आपूर्तिकर्ताओं को शामिल करके पर्यावरणीय प्रभाव को कम कर सकते हैं। डेटा-आधारित अपशिष्ट ऑडिट उच्च-उत्पादन लक्ष्यों की पहचान करते हैं। डिस्पोजेबल और पुन: प्रयोज्य वस्तुओं के बीच संतुलन बनाने के लिए एक विचारशील दृष्टिकोण की आवश्यकता होती है जो घुटने की आर्थ्रोस्कोपी के प्रभाव को कम करते हुए सुरक्षा बनाए रखे।
ट्रे संरचना को अनुकूलित करें और अनावश्यक वस्तुओं को कम करें।
विक्रेताओं के साथ मिलकर सामान वापस लेने या पुनर्चक्रण संबंधी पहल पर काम करें।
खरीद विकल्पों का मार्गदर्शन करने के लिए केस-स्तरीय अपव्यय पर नज़र रखें।
अभिसरण तेज़ी से बढ़ रहा है: रोबोटिक्स सटीक पोर्टल संरेखण में सहायता कर सकता है; एआई वास्तविक समय में ऊतक वर्गीकरण प्रदान कर सकता है; बायोप्रिंटिंग आर्थोस्कोपिक पोर्टल्स के माध्यम से कस्टम कार्टिलेज स्कैफोल्ड्स की डिलीवरी को सक्षम कर सकता है। अस्पताल इंटरऑपरेबल प्लेटफ़ॉर्म, निरंतर टीम प्रशिक्षण और सहयोगात्मक अनुसंधान को प्राथमिकता देकर भविष्य के लिए निवेश को सुरक्षित कर सकते हैं। सोच-समझकर कार्यान्वयन के साथ, घुटने की आर्थोस्कोपी कार्यक्षमता को बहाल करने, जोड़ों को संरक्षित करने और मूल्य-आधारित देखभाल को बनाए रखने में अपनी भूमिका का विस्तार करती रहेगी।
संक्षेप में, एक प्रभावी अस्पताल कार्यक्रम सुसंगत परिणाम देने के लिए प्रौद्योगिकी, प्रशिक्षण, संक्रमण नियंत्रण, डेटा प्रणालियों और रोगी-केंद्रित शिक्षा को एकीकृत करता है। नैदानिक लक्ष्यों को परिचालन उत्कृष्टता के साथ संरेखित करके, घुटने की आर्थ्रोस्कोपी एक प्रक्रिया से कहीं अधिक हो जाती है—यह उच्च-गुणवत्ता वाली आर्थोपेडिक देखभाल के लिए एक मापनीय ढाँचा बन जाती है।
अस्पतालों को उच्च परिभाषा इमेजिंग गुणवत्ता, एर्गोनोमिक उपकरण डिजाइन, नसबंदी संगतता और विभिन्न आर्थोस्कोपिक घुटने की सर्जरी प्रक्रियाओं के लिए अनुकूलनशीलता पर ध्यान केंद्रित करना चाहिए।
प्रतिष्ठित आर्थोस्कोपी निर्माता प्रमाणित सामग्रियों का उपयोग करते हैं, आईएसओ चिकित्सा उपकरण विनियमों का अनुपालन करते हैं, तथा विविध क्षेत्रीय और अस्पताल-विशिष्ट मानकों को पूरा करने के लिए कठोर परीक्षण करते हैं।
एक अनुभवी आर्थोस्कोपी आपूर्तिकर्ता समय पर डिलीवरी सुनिश्चित करता है, तकनीकी प्रशिक्षण प्रदान करता है, और अस्पताल के ऑपरेटिंग रूम वर्कफ़्लो में उपकरणों के एकीकरण का समर्थन करता है।
अस्पताल अक्सर सटीक घुटने की आर्थ्रोस्कोपी ऑपरेशन के लिए डिज़ाइन किए गए स्कोप, शेवर, द्रव प्रबंधन प्रणाली और प्रकाश स्रोतों सहित संपूर्ण आर्थ्रोस्कोपी सेट की मांग करते हैं।
वास्तविक समय में उच्च-रिज़ॉल्यूशन दृश्य प्रदान करके, घुटने की आर्थोस्कोपी सर्जनों को न्यूनतम ऊतक विघटन के साथ संयुक्त स्थितियों का आकलन और उपचार करने की अनुमति देती है।
रिकवरी का समय प्रक्रिया की जटिलता, रोगी की सर्जरी-पूर्व स्थिति और अस्पताल-आधारित फिजियोथेरेपी संसाधनों की उपलब्धता पर निर्भर करता है।
अस्पताल उत्पाद परीक्षण डेटा का अनुरोध कर सकते हैं, नसबंदी चक्र के परिणामों की समीक्षा कर सकते हैं, तथा पिछले चिकित्सा ग्राहकों से दीर्घकालिक प्रदर्शन रिपोर्ट की जांच कर सकते हैं।
निर्माता अस्पतालों को नए आर्थोस्कोपी उपकरणों को सुचारू रूप से एकीकृत करने में मदद करने के लिए उत्पाद प्रदर्शन, सर्जन प्रशिक्षण सत्र और तकनीकी सहायता प्रदान करते हैं।
कॉपीराइट © 2025.Geekvalue सभी अधिकार सुरक्षित।तकनीकी समर्थन: TiaoQingCMS